
A Guide for Navigating Long COVID Diagnosis and Treatment
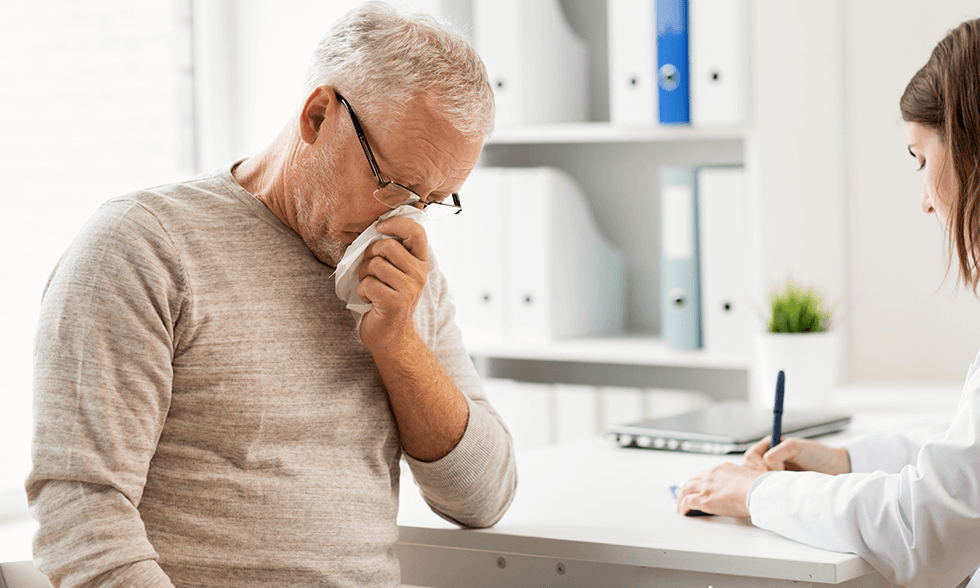
If you suffer lingering symptoms months after your initial COVID diagnosis, you’ve likely guessed that you’re experiencing what’s known as “Long COVID.” I know the road to recovery can feel long and lonely. Doctors are still learning about this condition and don’t know it well; treatment options remain limited. I don’t ascribe to that dismal view nor limit patient treatments to palliative care and emotional support. We can do better.
Don’t underestimate this condition. SARS-CoV-2 is a serious viral infection. So long-term, chronic consequences are expected, as with other viral diseases. The challenges of obtaining an accurate diagnosis and finding effective treatments for Long COVID symptoms cannot be understated. Many find themselves bouncing between specialists, undergoing a battery of tests, only to be told the results are inconclusive. It’s a frustrating process that requires patience, persistence, and self-advocacy.
The good news is that the medical community’s understanding of Long COVID is evolving. Thousands of researchers worldwide are working to comprehend the condition better, identify diagnostic markers, and develop targeted treatments. But for patients, it’s not fast enough.
Although the road ahead remains uncertain, resources are available to help you on your journey to recovery. That’s why I wrote this guide for navigating Long COVID
I organized this guide into several parts. The introduction provides an overview of the challenges in obtaining a Long COVID diagnosis and getting effective treatment from medical professionals. I aimed to strike an optimistic and encouraging tone for readers dealing with this condition but know all too clearly the clinical challenges chronic viral illness cause.
I’m not new to viral diseases. I’ve worked with patients with serious acute and chronic viruses for over thirty years. These included HIV before the discovery of AZT (azidothymidine), chronic HCV before Harvoni, chronic Epstein Barr Virus linked to ME/CFS and MS. And the H1N1 swine flu pandemic of 2009. I wrote two books on viral illness: Viral Immunity (2002) and Beating the Flu (2006).
From the standpoint of my work, the COVID-19 Pandemic was expected. So was Long COVID. In 2002-03, the first SARS (Severe Acute Respiratory Syndrome) emerged in Hong Kong and Guangzhou, China. Post-SARS was defined as ongoing symptoms, which were like Long COVID. But the number of cases was minor compared to the COVID-19 Pandemic. We should have paid more attention.
In November 2019, a few of my colleagues in China hinted at a new SARS-like illness in Hunan Province. By December, it became an office public health emergency. But it was not until March 11, 2020, after more than 118,000 cases in 114 countries and 4291 deaths, that the WHO declared pandemic status. More than four years later, we’re still getting sick from SARS-CoV-2. And a chronic form, Long COVID, emerged among survivors.
Introduction
Post-viral infection syndromes are not new to SARS-CoV-2 infection. In medical terms, post-viral illness generally refers to fatigue, ongoing tiredness, and weakness for weeks or months after the initial infectious reaction is gone.
A 1988 paper in the Postgraduate Medical Journal acknowledged that most patients who have had an acute infection pass through a stage of convalescence before they regain normal, active health. However, some progress to a chronic stage. We already saw it in Post-SARS. It was expected that some cases would become chronic. Long COVID is a chronic illness triggered by SARS-CoV-2 infection.
However, some cases have lingering symptoms that persist for months or years, and some develop permanent complications. Many have perplexing symptoms and signs that defy even the best diagnosticians. Unrelenting fatigue, that’s easily aggravated by mild activity, is the main symptom. Muscle aches and pains are another common complaint.
For decades, fatigue syndromes were disreputable. Doctors wouldn’t diagnose them, rather suggesting patients were depressed or malingering. This is how Chronic Fatigue Syndrome (CFS) was viewed initially after a cluster of cases appeared in Incline Village on Lake Tahoe in 1984.
I was a newly licensed clinician then and saw several of these cases at our group practice, Ecology Medical Clinic, in Del Mar, California. We didn’t have the tools to help most of them then, and I resolved never to be in that situation again. I committed my career to working hard to understand post-viral conditions and discover safe and effective treatments.
That’s why conditions like Long COVID are not new to me. Nevertheless, lots of questions remain. For example, are there any similarities between Mononucleosis and ME/CFS, one caused by EBV and the other associated with reactivated EBV infection? Is reactivation of EBV the cause of Long COVID? I intend to address these and other questions in this document.
Content Dashboard
The following are links to the seven main topics, or “chapters,” in this presentation about Long COVID.
- What Is Long COVID?
I define Long COVID in detail in this chapter and discuss the likely causes, symptoms, and clinical presentation. - A Summary of the Long COVID Research.
In this section, I review the different directions researchers have investigated and summarize what they found, making it relevant to helping you heal. - How Is Long COVID Diagnosed?
I review the basic clinical tests to determine ongoing viral illness, immune imbalance, and immune response to SARS-CoV-2 infection. I’ll also introduce advanced and experimental testing. - What Makes Long COVID So Hard to Understand?
In this chapter, we’ll look at the complexity of SARS-CoV-2 infection and its impact on the immune system and other body functions. - Conventional Treatment Options: What’s Most Likely to Work.
I’ll outline the recommended treatments and some controversial but evidence-based prescriptions here. - Alternative Therapies for Long COVID.
In this chapter, I’ll introduce natural therapies and nutritional supplements to bend the Long COVID curve. - Advanced and Experimental Treatments.
In the last installment, I present advanced immunological therapies used in Europe, including SOT and DendroCov Therapy. - Empowering Patients with Long COVID
Understanding strategies and tools to support and manage Long COVID patients effectively. - A 12-Step Plan to Beat Long COVID
I created a 12-Step Plan to Beat Long COVID. Some of it can be done on your own, and you can get started right now. Other aspects require a licensed healthcare professional. You may be already doing some of these, but if you suspect you have Long COVID, follow these steps. - CONCLUSIONS: Take Long COVID Seriously
The United States had the most cases of acute COVID. Nearly everyone got sick. But I didn’t because I took strict precautions early.
However, before exploring the details, let’s review the basics as a foundation for a more in-depth exploration of Long COVID.
Summary of Long COVID Basis
In this section, I summarize the conventional understanding of Long COVID. It’s a starting point for solving this post-pandemic crisis. Use it as a roadmap to orient yourself on your path to recovery.
However, don’t be passive. You must do more than give it time and exercise patience for longstanding and serious cases. Chronic health conditions usually don’t respond to time alone. You must put immunological pressure on the biological factors that cause persistent inflammation, immunological dysfunction, and metabolic imbalance. I call it being a proactive patient.
COVID GLOSSARY
· COVID-19 – Coronavirus Pandemic that started in 2019
· COVID – Coronavirus (CoV) Infectious Disease
· SARS – Severe Acute Respiratory Syndrome – the original SARS epidemic
· SARS-CoV-2 – SARS Coronavirus 2, the cause of COVID-19
. Long Covid – Also called Post Acute Sequalae of SARS-CoV-2 (PASC)
· Serelogy test – A laboratory study that identifies antibodies to determine the state of infection
Definition of Long COVID
Post-acute sequelae of SARS-CoV-2 infection (PASC), also known as Long COVID, is defined as ongoing, relapsing or new symptoms or conditions present three months or longer after the initial infection.
Long COVID has become a major clinical and public health concern. At least 10-20% of those infected with SARS-CoV-2 can develop long-term COVID complications. In the U.S., about 11% of acute COVID patients experience ongoing symptoms. That’s about 11 million cases. In the WHO European Region, that’s 17 million people. According to the Lancet, about 65 million worldwide have symptoms consistent with Long COVID.
Interestingly, though older patients are more likely to have serious complications of acute infection, older adults are less likely to have Long COVID. Women are more likely than men to develop long COVID symptoms. Though children and adolescents avoid the consequences of serious acute COVID, at least 10% develop symptoms of lingering illness consistent with Long COVID.
Diagnosing Long COVID: The Available Tests
To properly diagnose Long COVID, you need several tests and must answer a panel of questions. For example, did you get a rapid antigen test when you were initially sick or test positive for SARS-CoV-2 by other tests? Are the symptoms you experienced after acute COVID new? Or were you previously diagnosed with ME/CFS or other fatigue conditions?
The first step is a clinical assessment by your doctor to review your symptoms and medical history, followed by blood tests to check for signs of infection, inflammation, or organ damage.

Basic Blood Tests
Common blood tests for Long COVID include:
- Complete blood count (CBC) to check red and white blood cell counts for signs of anemia or infection. Be sure to get the CBC with a differential evaluation of the different types of white blood cells to check for immune deficiency.
- C-reactive protein (CRP) to detect inflammation in the body. Elevated CRP levels may indicate ongoing immune system activation.
- D-dimer to check for blood clots. Abnormal D-dimer levels could indicate potential clotting issues which require treatment.
- Cytokine panel to measure immune system messengers that regulate inflammation. Irregular cytokine levels may point to an overactive or underactive immune response.
I’ll discuss blood testing in detail in the chapter on diagneosis and evaluation.
Additional Clinical Studies
If blood tests are inconclusive or your symptoms warrant further investigation, your doctor can order the following studies:
- Chest computed tomography (CT) to check for lung inflammation or other respiratory system abnormalities.
- Echocardiogram (EKG) to examine heart function and look for signs of myocarditis, other heart damage, and irregular heart rhythm.
- Abdominal magnetic resonance imaging (MRI) or CT scan is used to detect organ inflammation or issues in the liver, gut, and other organs of the abdomen.
- Sleep study to diagnose potential sleep disorders exacerbating symptoms.
A key to properly diagnosing and treating Long COVID is ruling out other conditions and determining the severity and specifics of organ or system involvement. Ongoing monitoring and retesting may be required as symptoms change or evolve.
With the right diagnosis, an effective treatment plan can be developed to support your long-term recovery. I’ll go into advanced testing in a separate chapter.
Treatments for Long COVID Symptoms: What Works and What Doesn’t
While there is no cure for Long COVID, several treatments can help relieve your symptoms. Antihistamines and decongestants can reduce swelling and open airways for better breathing. Bronchodilators may provide relief from coughing and chest tightness. Steroid medications can reduce inflammation in the lungs and elsewhere but can mask underlying causes of inflammation, but they have profound side effects, including weight gain, intense mood swings, easy bruising, and slower wound healing.
Some doctors are repurposing drugs to target malfunctioning immune cells. These include maraviroc and pravastatin, investigated by Bruce Patterson. Paxlovid, the antiviral with some benefit against acute COVID, is repurposed for Long COVID. Low-dose naltrexone (LDN) has helped some patients. Metformin, an anti-diabetes drug, may benefit the metabolic aspects of Long COVID. I’ll go over these and other medications in detail in Chapter 5.

Supplemental oxygen or respiratory therapy may be options if your oxygen saturation levels are low. Oxygen saturation is measured using a finger clip oximeter for specific oxygen (SpO2). A normal SpO2 is 95% or higher. A SpO2 of less than 90% saturation is considered dangerous.
Resting helps, but no matter how much you rest, the underlying cause of Long COVID makes symptoms persist, despite extra rest. That’s also part of the problem with ME/CFS. You feel worse with activity, but resting is not a cure.
Pacing your activities and getting extra rest is important for managing fatigue and shortness of breath. Physical therapy or occupational therapy may improve endurance and make daily tasks easier. Tai qi and Qigong practice improves airways and increases oxygen saturation.
Speech or cognitive behavioral therapy could help with neurological or cognitive symptoms. Headaches, dizziness, or insomnia may be treated with medication or lifestyle changes. Stomach issues could require diet changes, probiotics, or medication.
Alternative Therapies for Long COVID
Some people have found relief from alternative therapies like acupuncture, massage therapy, or yoga. Although there is little evidence of their effectiveness for Long COVID, many patients benefit from these therapies. I’ll discuss acupuncture’s effect on regulating the vagus nerve and how it re-establishes a healthy, balanced nervous system in Chapter 6.
Finding and implementing the right treatment plan can take time and persistence. You may need to try various options to determine what helps and be flexible as your condition changes. Discuss all treatment ideas with your doctor to ensure safety and effectiveness. While recovery can feel painfully slow, many people experience gradual improvement over weeks and months. Slow progress is better than no progress. You can navigate this difficult journey toward better health and functioning by focusing on self-care, pacing yourself, and working closely with your medical team.
Daily Management of Long Covid Fatigue and Some Safe Ways for Improving Energy Levels
Managing the fatigue and low energy that comes with long COVID can be challenging. However, there are several steps you can take to improve your energy levels.
- Stay hydrated and eat a healthy diet. Drinking plenty of water and other fluids like herbal teas helps avoid dehydration, which can worsen feelings of fatigue. Keep up with electrolytes, which you can add to your water, or drink fresh vegetable juices.
- Focus on nutritious, balanced meals with lean proteins, high-fiber whole grains, fruits, and vegetables. Limit excess sugar, salt, alcohol, and caffeine.
- Get extra rest. Long COVID often causes severe fatigue and exhaustion. Try to get 9-10 hours of sleep per night and take short naps during the day if needed. Resting will help your body heal.
- Pace yourself and avoid overexertion. Start slow and listen to your body. Only do light activities and exercises that you can tolerate. Pushing yourself too hard can make symptoms worse. Learn to balance activity and rest.
- Try relaxation techniques. Practicing mindfulness, meditation, deep breathing, yoga, or Tai Chi may help decrease stress and boost energy levels. Reducing stress is important for recovery and symptom management.
Medications May Help, But Don’t Cure
Discuss medication options with your doctor. Certain medications may help reduce inflammation, improve oxygen levels, or stimulate energy production at the cellular level. However, more research is needed to determine optimal treatments. Your doctor can determine if medication, nutritional supplements, or other therapies may benefit you based on your unique symptoms and health profile.
Rehabilitation and Physical Therapy Options for Long COVID Patients
For Long COVID patients, rehabilitation and physical therapy can play an important role in recovery. Under the guidance of a physiatrist and physical therapists, certain exercises and therapies may help improve symptoms and quality of life.
Physical Therapy
Physical therapy focuses on improving mobility, flexibility, and strength. A physical therapist can tailor a personalized exercise plan for Long COVID patients based on individual symptoms and limitations. Some options may include:
- Aerobic exercise like walking or light cardio improves endurance and stamina. Start slowly and build up duration and intensity over time as tolerated.
- Strengthening exercises targeting major muscle groups. The use of resistance bands or very light weights may be options as strength improves.
- Stretching and range-of-motion exercises to increase flexibility and mobility. Yoga or Tai Chi for balance may be suitable for some patients.
- Postural exercises to improve balance, coordination, and correct muscle imbalances from prolonged inactivity during illness.
- Breathing exercises like diaphragmatic breathing can maximize lung capacity and oxygen levels. Simple meditation practices can reduce stress and create a positive outlook for the future.
Occupational Therapy and Rehabilitation
Occupational therapy aims to improve patients’ daily activities and independence skills. An occupational therapist can evaluate limitations and provide strategies to help with:
- Task planning, prioritizing, and organization around home and work responsibilities
- Memory aids and reminders for important activities or events
- Energy conservation techniques like resting before tasks, using mobility aids like a cane for better balance and preventing falls, and streamlining routines.
- Stress and anxiety management through relaxation, mindfulness, and flexible coping strategies
Rehabilitative therapy provides Long COVID patients a path forward to regain strength, endurance, independence, and an improved quality of life. With time and consistency, many patients experience gradual yet meaningful improvements in their condition. Patients should discuss options with their physicians to determine the most beneficial therapies based on individual symptoms and needs.
Functional Medicine Approaches for Long COVID
Functional medicine takes a holistic approach to treating Long COVID by addressing the root causes of symptoms. Some approaches to explore include:

Dietary Changes
Adjusting your diet to include fresh vegetables and juices can help reduce inflammation in the body and support your immune system. An anti-inflammatory diet emphasizes whole foods like fruits and vegetables, lean proteins, and whole grains while limiting processed foods, sugar, and red meat. Intermittent fasting, reducing intake to an 8-hour window each day, may also help. Drink plenty of water to stay hydrated,

Stress Reduction
Chronic stress taxes your immune system and adrenal glands, worsening Long COVID symptoms. Engage in regular stress relief like light exercise, meditation, yoga, or deep breathing. Limit screen time and social media, which can be overstimulating. Get 7-9 hours of sleep per night to allow your body to rest and recover. Consider seeing a therapist who can provide coping strategies tailored to your unique situation.

Guided Imagery
Guided imagery is a science-based meditation that may include positive affirmations. It’s a way of changing a sickness mindset of hopelessness and victimization to hope and healing using positive thinking and words that re-balance the autonomic nervous system. Guided imagery and meditation can have profound effects on restoring health.
Light Exercise
While rest is important initially, light activity and exercise provide benefits when you can. Take short walks, do gentle yoga, use resistance bands for strength training, or try Tai Chi. Start slowly and build up endurance over weeks and months. Exercise increases blood flow, releases endorphins to improve mood, and strengthens your body. However, be careful not to overexert yourself, which can worsen symptoms.
Nutritional Supplement Support
Certain supplements may help address nutritional deficiencies, reduce inflammation, and support your immune system and adrenal glands. However, you should always talk to your doctor before starting any supplement regimen for Long COVID. They can help determine what may be right based on your unique symptoms and health history. Common supplements for Long COVID include Vitamin C, D, zinc, NAC, CoQ10, turmeric, and fish oil which has anti-inflammatory effects. To reduce potential allergic sensitivity to fish oil, I recommend Krill oil.
I’ll provide in-depth supplement advice in the chapter on natural medicine.
Integrative Therapies and Advanced Immune Treatments

Natural therapies have a therapeutic part and play palliative roles in managing the course of Long COVID and nudging the body toward healing. These include herbal medicine, homeopathic remedies, bioregulatory medicines, acupuncture, intravenous blood irradiation, and ozone treatments.
Advanced immune therapies include SOT and DendroCov from RGCC Laboratories. RGCC scientists are experts in personalized testing for drugs and natural substances used for cancer. They also developed immune-based therapies for chronic viral infections, including SARS-CoV-2. RGCC’s laboratories use the patient’s isolated monocytes as a source for the in vitro production of dendritic cells to produce an individualized vaccine. The goal is to stimulate the patient’s immune system against the virus. I discuss these in Chapter 7.
Navigating Long COVID Diagnostics: A Patient’s Perspective
Navigating the twisting road to a Long COVID diagnosis and finding proper treatment can be frustrating and disheartening. The process can feel opaque and convoluted. However, by understanding the diagnostic steps, you can advocate for yourself and work with your doctors to find answers and relief.
Your physician will evaluate your medical history, symptoms, and timeline to determine if your symptoms match those of Long COVID. They will attempt to rule out other possible conditions or causes through blood tests, imaging scans, and other procedures that cause similar symptoms. Common diagnostics for Long COVID include:
- Blood tests to check for signs of inflammation, autoimmune responses, or other abnormalities.
- Chest CT scans or X-rays to check for lung inflammation or other damage.
- Brain MRIs check for changes related to brain fog or other neurological symptoms.
- Heart tests like EKGs or echocardiograms check for damage or inflammation.
If all other possible diagnoses are ruled out, but your symptoms persist, your doctor may determine you have post-acute COVID-19 syndrome, known as Long COVID. From there, finding adequate treatment is challenging and often requires patience during the trial-and-error process. We can do better. That’s why I wrote this guide.
In summary, making targeted lifestyle changes and exploring natural therapies under the guidance of an experienced doctor can help support your body’s healing from Long COVID. While recovery may be slow, functional medicine approaches aim to restore balance and build resilience over time.
Conclusion

While recovering from chronic COVID can be a long road, focusing on self-care, pacing your activities, and making healthy lifestyle changes will help you regain your strength and vitality over time. Be patient and compassionate with yourself during this difficult process. With the support of your medical team, family, and community, you can start to feel more like yourself again.
The road to recovery from Long COVID may seem never-ending, so it’s called “long.” However, by working closely with your doctors to determine an accurate diagnosis and find a suitable treatment plan, you can start feeling better and reclaim your health.
Be your own best advocate, do your research, and don’t give up hope. Many Long COVID patients begin to heal with time and the right treatment.
Remember to be patient and kind to yourself as you continue recovering from Long COVID. Listen to your body’s needs, take things slowly, and prioritize your health and well-being when planning daily activities. Reach out to your doctor or support group when you need help. Connecting with others experiencing similar health issues can help reduce feelings of isolation and provide practical advice and emotional support. Continue advocating for yourself to find the right treatment and care team.\
Though the road ahead remains uncertain, stay focused on each day as it comes. Celebrate small milestones and little victories and maintain hope that ongoing research will lead to improved diagnosis and more effective treatments.
You have overcome much to get here, so keep putting one foot before the other. Brighter days are ahead. Never give up.
In the individual chapters, we’ll deeply dive into ways to beat Long COVID.
Here To Help
If you are a “long hauler” experiencing symptoms of Long COVID, we can help. You’ll start with comprehensive testing to understand your immune status and establish a baseline of overall health. The first therapeutic goal is controlling symptoms, followed by a comprehensive treatment and management plan to support your respiratory and immune health long-term.
Contact Dr. Williams:
Contact Our Clinic
Florida Integrative Medical Center
2415 University Pkwy, Suite 218, Sarasota, FL 34243