How Is Long COVID Diagnosed?
There are several tests for acute COVID but no definitive test for Long COVID. How can you tell if you have Long COVID?
CONTENTS:
Tests for SARS-CoV-2 Infection

You performed a rapid antigen test at home when you first experienced symptoms, and it returned positive. Most likely, you were exposed to the virus at work, so you promptly self-quarantined at home. Your symptoms persisted, with a fever, cough, and sore throat lasting several days. You felt weak and tired, prompting you to schedule a 15-minute online visit with your doctor. During the virtual consultation, your doctor ordered tests for active infection by reverse transcription polymerase chain reaction (RT-PCR), the gold standard for confirming active SARS-CoV-2 infection. The results came back positive, and your doctor prescribed Paxlovid, which helped your fever go down. However, it’s been over a month, and you still have swollen lymph glands and are tired and weak even with rest. Are you in the early stages of Long COVID? You want to know more about your condition; proper testing may provide some insights. But there’s no specific test for Long COVID. How do you work around the lack of testing?
Rapid tests can detect immune activity after exposure, even if you don’t have symptoms. Rapid tests and RT-PCR tests are used to diagnose acute COVID infection, with positive results confirming the infection. Your healthcare provider can order the RT-PCR test for you, and in some cases, you can obtain these tests online without a doctor’s lab requisition. In either case, you’ll need to provide a blood sample at the lab’s draw station, or a mobile phlebotomist can visit your home or business.
Quest Diagnostics: Initially, you want to know if you have an active infection. Quest Diagnostics uses the RT-PCR/TMA (SARS-CoV-2 RNA, QL NAAT) test. If you suspect you had an active infection and want to know your level of immune response, you’ll also need the SARS-CoV-2 Antibody (IgG), Spike, Semi-Quantitative test.
Quest Diagnostics also offers a Post COVID-19 Expanded Panel. However, this panel doesn’t provide insight into acute or chronic viral infection. Instead, it offers an overview of your general health and how you’re coping with a lingering infection. Unfortunately, it doesn’t provide specific insights into the chronic viral effects of Long COVID.
Labcorp: This national lab provides the same COVID tests as Quest, including SARS-CoV2-Semi-Quantitative IgG Antibody, Spike, and others. It also offers a Long COVID profile with more tests than the Quest panel, but it’s still very limited in explaining chronic illness associated with COVID.
VibrantAmerica: This specialty lab provides an infection cycle profile. These are the same tests as the national labs, but Vibrant charts the results to make understanding your post-infection status easy. If your IgM is negative, but your IgG is very high eight weeks or more after initial infection you likely still have lingering effects from infection.
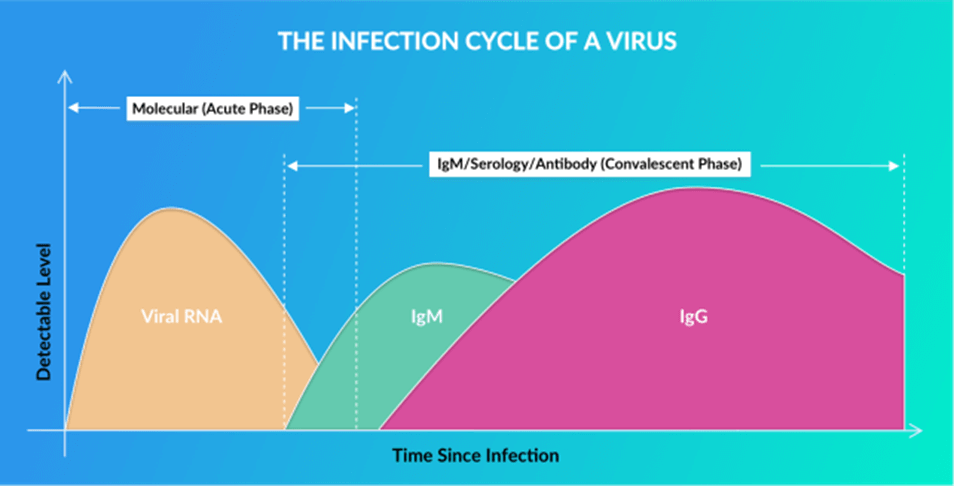
Acute, early disease occurs within 0-14 days after infection. That’s when viral RNA is present and you’re contagious. IgM Antibody (Ab) tests show positive results from 1-8 weeks after infection. IgM is the immune system’s frontline response during the early infectious stage. IgG Ab appears when the body mounts a long-term immune response that may last months or even longer. A persistently high IgG is associated with chronic infection, as found in the early stages of Long COVID. You can use a sample from serum or a dried blood spot on a blotter from a finger prick, the type you can easily do at home, making it a safe and convenient option. However, so far, none of these labs has a definitive test for Long COVID.
Looking for Patterns in Diverse Biomarkers
Clinicians and researchers understand the absence of a definitive Long COVID marker makes diagnosis difficult. Nevertheless, that doesn’t prevent them from looking at available tests for immunological insights as a guide for likely disease. Even though there’s no definitive test to determine Long COVID, your doctor can look for patterns found in various tests to size up your body’s response to SARS-CoV-2 infection and gain insight into your overall health and immune status. These markers offer a pathway for understanding the body’s response to chronic infection and immune disruption following SARS-CoV-2 infection. However, interpreting the results requires the expertise of a clinician skilled in viral immunity.
Comprehensive List of Blood Tests for Health Conditions Associated with Long COVID:
- Apolipoprotein A and E
- B-cells
- Brain natriuretic peptides (BNP)
- Calprotectin
- CD40LG
- Creatine kinase (CK)
- Complete blood count (CBC) with differential
- Comprehensive metabolic panel (CMP 14)
- C-reactive protein (CRP)
- Cystatin-C
- D-dimer
- Erythrocyte sedimentation rate (ESR)
- Ferritin
- Fibrinogen
- Interleukin 2 (IL-2)
- Immunoglobulin profile, quantitative IgA, IgE, IgG, IgM
- Immunoglobulin G, subclasses 1-4
- Iron and total iron-binding capacity (TIBC)
- SARS-CoV-2 Antibodies IgG and IgM
- T- and -B lymphocyte count with natural killer cells
- Tumor necrosis factor alpha (TNF alpha)
- Troponin
- Vascular endothelial growth factor (VEGF)
- Vitamin B12
- Vitamin D, 25-hydroxy
- Vitamin K2
This is a broad list of lab tests associated with health and response to infection. Not every Long COVID patient requires all of them. The choice of tests depends on how comprehensively you and your doctor wish to conduct the examination and the specific objectives your doctor wants to address. Here are some ways to organize your results.
Long COVID symptoms appear in clusters. For example, is the diagnostic focus on an inflammation cluster, an immune response imbalance, or an immune deficiency cluster? Other concerns include clotting issues and gut-brain microbiome disruption. While this is a very challenging condition, grouping tests can assist in understanding what drives your symptoms and provide guidance for your Long COVID care.
3 Diagnostic Categories
· CRP
· Ferritin
· IL-2
· TNF alpha
2) Immune Imabalce
· CBC with differential Immunoglobulin Profile T-and-B Lymphocytes
3) Immune Deficiency
· CBC with differential Immunoglobulin G, subclasses T-and-B Lymphocytes
Additional Markers:
NLR: The neutrophil-to-lymphocyte ratio (NLR) was used early in the COVID-19 pandemic to predict disease severity and mortality in acute infections. A high NLR is associated with more severe cases. Since it’s a mathematical calculation, you can easily do it by dividing your total neutrophils by lymphocytes. An NLR of greater than 3.3 indicates more severe infection. However, few studies link NLR as a predictor for Long COVID or its severity. Neutrophils and lymphocytes are white cell types found on a CBC with Differential and Platelets panel. Labcorp offers a COVID-19 Severe Disease Progression Risk Profile that includes these markers and an NLR calculation.
PLR: The platelet-to-lymphocyte ratio (PLR) is another calculated marker for predicting acute disease severity and mortality in COVID patients. A 2023 study suggested that the NLR and PLR represented markers of indirect inflammation that were higher in the Long COVID study patient group.
ANA: Antinuclear antibodies (ANA) can help you learn if you have an autoimmune disease versus an infection. Since many autoimmune conditions share symptoms with Long COVID or can trigger it, getting an ANA test is a starting point to rule out autoimmune activity.
Note: To be clear, COVID is not an autoimmune disease. Nonetheless, an overly aggressive immune response to the virus or a vaccine can have harmful effects like those seen in autoimmune conditions. Some doctors believe autoimmunity is one of the critical causes underlying Long COVID symptoms. Get the ANA test.
Immunoglobulin Deficiency Signature With Low IgM and Low IgG3: Decreased immunoglobulin M (IgM), a marker for acute infection, is sometimes found in patients during primary infection and up to six months later. Additionally, research found that total immunoglobulin G3 (IgG3) levels were lower in post-infection cases. During the post-infection stage, patients with low IgM or high IgG levels may have an increased risk for Long COVID. Those with both low IgM and low IgG3 levels have an immunoglobulin deficiency that may accompany Long COVID.
Tests for Overlapping Chronic Infections: SARS-CoV-2 can reactivate Epstein Barr Virus (EBV) or Lyme Disease. Research suggests that reactivation of EBV increases the risk of developing “brain fog.” If you’ve had these infections in the past and are currently experiencing similar symptoms, it’s wise to update your immune status to EBV and Lyme. Joseph Burrascono MD, a tick-borne disease specialist, believes that Long COVID is a reactivation of Lyme.
Advanced Blood Markers: Your family doctor or general practitioner is unlikely to order these advanced tests. However, immunologists are familiar with and utilize these tests to assess immune status in response to infection. Discuss the advantages of these tests with your Long COVID specialist if you have severe or lingering symptoms lasting over six months.
- Atypical Monocytes – Researchers found irregular monocytes in COVID patients with lasting breathlessness after infection. Monocytes, a type of white blood cell tested in the complete blood count with differential, play various roles during infection and tissue repair. In comparison to healthy individuals, Long COVID patients have monocytes with different levels of proteins attached to them, which are critical for directing the cells toward the lungs. These results, scientists think, link abnormal monocytes with Long COVID and lung injury.
- Dysregulation of B–Cells – Abnormal B-lymphocyte activity during and post-infection may explain the presence of autoimmunity in Long COVID. A T- and -B lymphocyte Count with Natural Killer Cell profile during initial testing is recommended.
IncellDx: Scientists using advanced precision laboratory methods found blood markers that are consistently abnormal in long haulers. Using a mathematical model, they developed an algorithm of 97% accuracy in predicting non-severe and severe causes of Long COVID. IncellDX formally launched testing services in Europe in 2022 and the UK in early 2023. IncellDX is also available in the US, with IncellDx being marketed as 90% accurate.
Bruce Patterson, MD, an early and outspoken pioneer in proactive COVID infection treatment, has shifted his focus to Long COVID. Patterson believes that chronic inflammation in the blood vessels is the common factor in Long COVID as well as in other chronic post-infection syndromes like ME/CFS and Lyme. He is actively involved in bringing IncellDx to US patients.

Is There a Long COVID Microbiome?
A disruption of the gut-brain axis is suspected in the persistent neurological symptoms of ME/CFS and Long COVID. In 2020, researchers discovered that the virus particles responsible for respiratory tract illness can also infect the gastrointestinal (GI) tract, including the esophagus, stomach, small intestines, and colon. This can trigger GI symptoms such as abdominal pain and diarrhea, which usually improve as individuals recover. However, in some Long COVID cases, these symptoms persist. Laboratories in Hong Kong and Norway have developed gut microbiome testing for Long COVID, but these tests are not yet available in the US.
Long COVID Diagnosis Summary
Testing for acute and chronic SARS-CoV-2 virus infection is available from standard reference labs, including Quest Diagnostics, Labcorp, ARUP, and specialty laboratories like VibrantAmerica. The ideal test would detect immune markers specific to Long COVID, differentiating it from other diseases with similar symptoms such as EBV or Lyme. However, as of now, there is no specific test for Long COVID in the US.
A diagnosis of Long COVID is based on a laboratory confirmed COVID infection and the presence of specific symptoms persisting for more than four weeks after the initial infection. The National Institutes of Health (NIH) defines Long COVID as symptoms persisting for more than three months following the initial infection. These symptoms are characterized by their chronic nature, cycling between milder and more severe forms but rarely going away.
Although no specific laboratory test defines Long COVID, your doctor can gain insight into your body’s immunological response, or lack of activity, to SARS-CoV-2 infection by ordering several different clinical blood tests.
Dr. Williams’ Recommended Long COVID Basic Test Panel:
- Complete Blood Count with Differential
- Comprehensive Metabolic Profile 14
- C-Reactive Protein, highly sensitive
- D-dimer
- Total IgM, IgG
- Immunoglobulin G Subclasses Panel
- T and B Cells, total
Additional testing may be necessary to rule out overlapping illnesses or reactivated chronic viruses, including EBV VCA Antibody IgM, IgG, and EBV Nuclear Antigen (EBNA). A microbiome stool test identifies whether your gut serves as a reservoir for SARS-CoV-2 RNA viral infection that continuously reinfects or triggers immune activity.
You won’t necessarily need all these tests. Instead, the focus is on identifying critical immune activity to target treatments effectively.
In my practice, I begin establish a chronological history, starting with likely SARS-CoV-2 exposure and the date of the original acute symptoms. Then, I review the patient’s previous test results and identify a clinical pattern of symptom clusters. Based on this evaluation, I order additional tests as necessary. Finally, I consolidate all the clinical information to develop a treatment strategy, which I’ll discuss in the following chapters.
Selected References & Resources
Amruta Pise, Hallison Rodrigues, Purvi Parikh, Javier Mora, Rodrigo A Mora-Rodríguez. bioRxiv 2020.12.16.423122; doi: https://doi.org/10.1101/2020.12.16.423122
Asperges E, Albi G, Zuccaro V, Sambo M, Pieri TC, Calia M, Colaneri M, Maiocchi L, Melazzini F, Lasagna A, Peri A, Mojoli F, Sacchi P, Bruno R. Dynamic NLR and PLR in Predicting COVID-19 Severity: A Retrospective Cohort Study. Infect Dis Ther. 2023 Jun;12(6):1625-1640. doi: 10.1007/s40121-023-00813-1. Epub 2023 May 17. PMID: 37198387; PMCID: PMC10191087.
Bruce K Patterson, Jose Guevara Coto, Ram Yogendra, Edgar Francisco, Emily Long,
Cervia, C., Zurbuchen, Y., Taeschler, P. et al. Immunoglobulin signature predicts risk of post-acute COVID-19 syndrome. Nat Commun 13, 446 (2022). https://doi.org/10.1038/s41467-021-27797-1
Clemente I, Sinatti G, Cirella A, Santini SJ, Balsano C. Alteration of Inflammatory Parameters and Psychological Post-Traumatic Syndrome in Long-COVID Patients. Int J Environ Res Public Health. 2022 Jun 9;19(12):7103. doi: 10.3390/ijerph19127103. PMID: 35742355; PMCID: PMC9222533
Deeks JJ, et al; Cochrane COVID-19 Diagnostic Test Accuracy Group. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst Rev. 2020 Jun 25;6(6):CD013652. doi: 10.1002/14651858.CD013652. Update in: Cochrane Database Syst Rev. 2022 Nov 17;11:CD013652. PMID: 32584464; PMCID: PMC7387103.
Fedorchenko Y, Zimba O. Long COVID in autoimmune rheumatic diseases. Rheumatol Int. 2023 Jul;43(7):1197-1207. doi: 10.1007/s00296-023-05319-0. Epub 2023 Mar 30. PMID: 36995436; PMCID: PMC10061411.
Hashimoto, K. (2023). Detrimental effects of COVID-19 in the brain and therapeutic options for long COVID: The role of Epstein–Barr virus and the gut–brain axis. Molecular Psychiatry, 1-9. https://doi.org/10.1038/s41380-023-02161-5
Iosef C, Knauer MJ, Nicholson M, Van Nynatten LR, Cepinskas G, Draghici S, Han VKM, Fraser DD. Plasma proteome of Long-COVID patients indicates HIF-mediated vasculo-proliferative disease with impact on brain and heart function. J Transl Med. 2023 Jun 10;21(1):377. doi: 10.1186/s12967-023-04149-9. PMID: 37301958; PMCID: PMC10257382.
Nicholas A. Scott, et al. European Respiratory Journal Jan 2023, 2202226; doi: 10.1183/13993003.02226-2022
Thompson, J. S., Thornton, A. C., Ainger, T., & Garvy, B. A. (2022). Long-term high-dose immunoglobulin successfully treats Long COVID patients with pulmonary, neurologic, and cardiologic symptoms. Frontiers in Immunology, 13. https://doi.org/10.3389/fimmu.2022.1033651
Toori KU, Qureshi MA, Chaudhry A, Safdar MF. Neutrophil to lymphocyte ratio (NLR) in COVID-19: A cheap prognostic marker in a resource constraint setting. Pak J Med Sci. 2021 Sep-Oct;37(5):1435-1439. doi: 10.12669/pjms.37.5.4194. PMID: 34475926; PMCID: PMC8377926.
Woodruff, M.C., Ramonell, R.P., Haddad, N.S. et al. Dysregulated naive B cells and de novo autoreactivity in severe COVID-19. Nature 611, 139–147 (2022). https://doi.org/10.1038/s41586-022-05273-0
About J. E. Williams, OMD, FAAIM
Dr. Williams is a highly respected integrative medicine clinician who treats and revitalizes patients with even the most severe stages of illness. His mission is to bridge complementary and alternative therapies with evidence-based clinical science. His integrative practice offers proven natural therapies, including acupuncture, regenerative therapies, advanced intravenous ozone, blood irradiation, personalized natural therapies, and nutritional supplements. Dr. Williams is the author of Viral Immunity and Beating the Flu.
Learn More:
Our team of experienced functional medicine practitioners, medical doctors, and licensed clinical support staff are compassionate and knowledgeable in the diagnosis and treatment of chronic viral infections, including Long COVID. We have extensive experience treating Lyme disease, chronic EBV, and supporting viral immunity.
Contact Our Clinic
DaSilva Institute
3131 South Tamiami Trail Suite 202
Sarasota, Florida 34239
(941) 388 0940