CONCLUSIONS: Take Long COVID Seriously
SARS coronaviruses cause severe, often fatal infections. Acute SARS-CoV-2 is a severe infection that caused COVID-19, a historical viral pandemic like the 1018 Influenza Pandemic. It’s not surprising that a chronic form, Long COVID, persists well after the acute stage has passed.
Compared to other viral infections, a 2020 New York Times article reports that only 0.1% die from the flu annually. The fatality rate from the 1918 Influenza Pandemic was 2%. In a 2024 paper, the WHO called the COVID-19 Pandemic a “universal catastrophe.” About 3.4% of those infected with the SARS-CoV-2 virus died.
On April 4, 2024, The Economist published an executive summary about Long COVID, updating estimated deaths worldwide. Russia fared the worst, followed by other Eastern European countries. Britain had the highest per capita death count in Western Europe, earning it the name “Plague Island.” A 2024 article in the Guardian estimates that 2 million people have Long COVID, and many of these have had symptoms for more than two years.
The United States had the most cases of acute COVID. Nearly everyone got sick. But I didn’t because I took strict precautions early, starting in late December 2019. Other than going to the clinic, I stayed home. When I went out, I wore a face mask before it became policy. I supported my immune system by taking supplements, including zinc, selenium, beta-glucan, and vitamin C. And I never missed a day in the clinic. I went to work as usual. I created exacting policies for staff and providers at our clinic, and everyone complied. A few of our workers got sick outside of the clinic, but no one got sick from exposure at our clinic. And no one, except myself, developed Long COVID.
The Long Tail of the Pandemic
The consequences of the COVID-19 Pandemic will be long-lasting. Besides physical symptoms like muscle aches, behavioral impacts include sleep difficulties, a decreased sense of safety, irritability, alcohol abuse, overuse of tobacco, and over-dependence on prescription medications, along with interpersonal conflict, which is a short list of physical and psychological responses to this disaster.
Think of it as a tornado with a very long tail. There’s the dramatic tearing apart of structures, but the psychological impact will linger for a long time, profoundly impacting the mental and emotional well-being of the population. And the economic impact will be felt for years to come. We need reminders of hope now and ongoing encouragement along the way back to normal. Be patient. It will take time, but we’ll get there.
Long COVID is the most publicized aspect of the post-pandemic long tail. A 2024 Scientific American article states that the incidence of Long COVID is about 11 percent among the unvaccinated and 5 percent among those with two or more vaccine doses. That’s about 200 million people worldwide who have Long COVID—a catastrophic number.
However, statistics don’t reflect individual human misery. No common medical framework accurately describes Long COVID or provides a model of effective therapies, which I attempt to do in this book. The focus, as you would expect, is on prevention. Conventional medicine relies on vaccination as the primary preventive measure. However, this chronic condition is challenging doctors because there is no standard agreement among healthcare providers and public health professionals about the nature of Long COVID or the most effective prevention and management methods, and nobody claims to have a cure. Vaccination is helpful but not perfect.
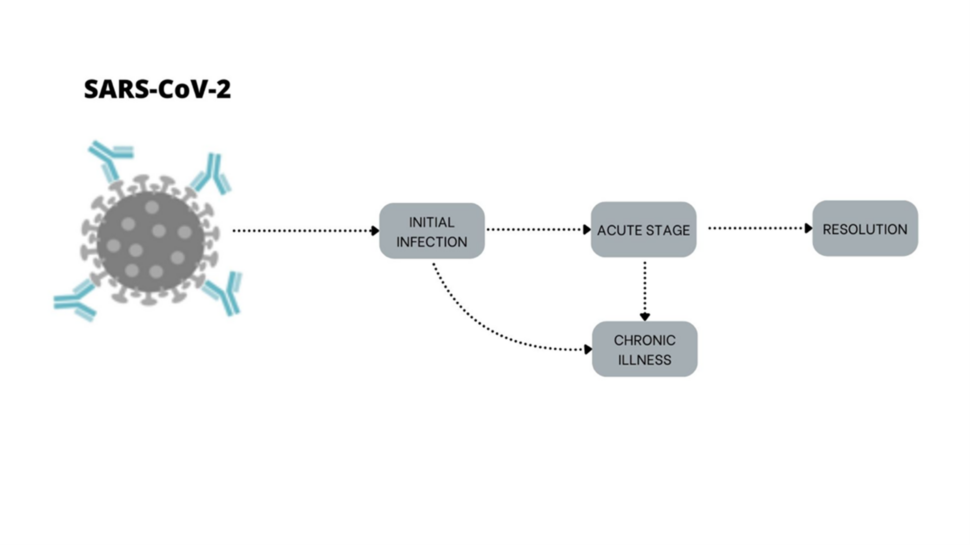
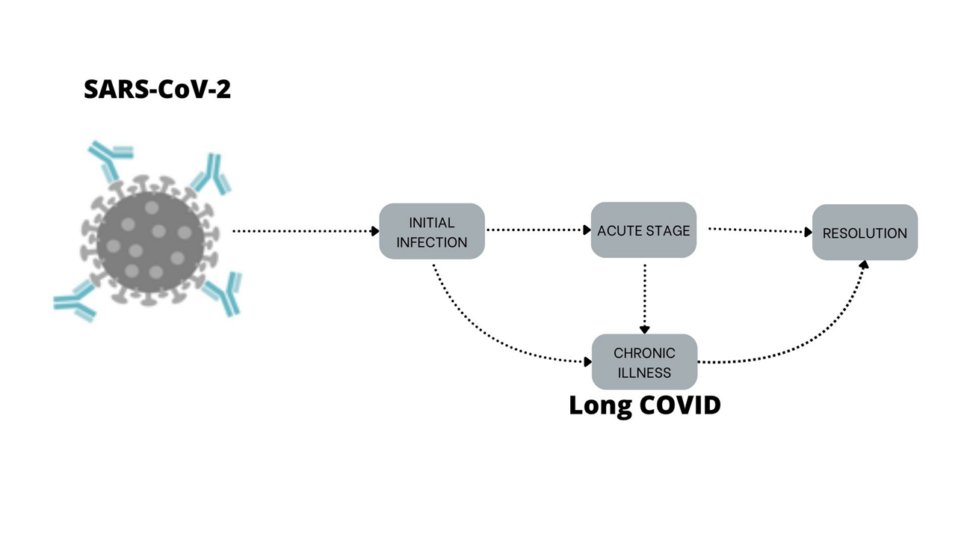
The Natural Course of Infection From SARS-CoV-2 To Long COVID
The natural course of infection from SARS-CoV-2 follows a predictable pathway. Exposure to the virus results in an initial infection progressing to the acute symptomatic stage. Most acute cases resolve on their own within a few weeks. Paxlovid helps for some. Zinc, selenium, and vitamin C can help prevent infection, reduce symptoms, and speed recovery. But some don’t get better; symptoms linger and progress to a chronic stage. Some bypass the acute stage, going directly to the chronic form of Long COVID.
SARS-CoV-2 infection is yet another in a growing number of viral infections that leave long-term conditions that are poorly understood and inadequately treated. These include AIDS, chronic hepatitis C, chronic encephalitis from measles, Dengue fever, and CFS from Epstein-Barr virus. We have drugs that manage AIDS and chronic hepatitis. However, an effective care model for Long COVID is not yet available. Of course, effective treatment and prevention during acute infection can reduce the total number of new cases. However, treatment models are lacking for those who remain sick.
New COVID Variants
According to a Scientific American article, SARS-CoV-2 continues to mutate. That’s no surprise because that’s what viruses do. A new group of Omicron variants, FLiRT, is circulating in the U.S. The acronym refers to amino acids that make up the protein spike so notorious in the virus’s composition. This new FLiRT group is part of the Omicron family and has multiple variants, including KP1.1, KP.2, and KP.3. Current vaccines are less effective against KP variants.
Researchers and doctors keep comparing COVID to seasonal influenza. That’s a hopefulness that doesn’t line up with viral biology. It’s a more serious respiratory infection than the flu. And there is a gut-lung interaction, making it more complex. We’ve gotten better at managing acute COVID infections, but it’s still potentially deadly. However, we haven’t found an effective way to cure or manage Long COVID.
True, deaths have been way down in the last few years. But don’t let the past few months’ lower level of infectious activity lure you into complacency. COVID has not gone away. Symptoms of the new variants are like those caused by JN.1, including loss of sense of taste or smell. The potential for severe infection is high because current vaccines are ineffective against the FLiRT variants, and natural immunity from infections from previous variants may not work against KP.2.
The same precautions apply: avoid exposure, wear a face mask, have COVID rapid tests on hand, and take the essential immune-supportive supplements.
A Multidisciplinary Model for The Treatment of Long COVID
A multidisciplinary approach involving several treatments may be more beneficial than a drug or a pharmaceutical cocktail. When using a combination of different therapies simultaneously to treat a disease, it’s best to rely on natural medicines and nutritional supplements, lifestyle interventions including adequate rest, and meditation or visualization. These interventions support body functions and have fewer adverse effects.
Somatic mind-body techniques can be transformative. These include yoga postures, emotional release techniques, and Taichi. Acupuncture can play a central role due to its ability to regulate the balance of the parasympathetic and sympathetic nervous systems, the gut-brain axis, and the immune system. It also has an overall effect on promoting well-being.
Revisiting Vaccination and Long COVID
I didn’t get acute COVID. My brush with Long COVID came from my second Pfizer vaccination. Let me be clear: I’m neither an anti-vaxxer nor do I support vaccination for every infectious illness for everyone. After all, you won’t get sick if you don’t get exposed. The best protection is not to get infected. But I know we can’t live in a bubble. So, I recommend vaccination for my patients. However, we can be more proactive; we can minimize exposure. We can take immune-supportive supplements. But is it always practical?
If you don’t get acute COVID, you can’t get Long COVID. However, not everyone who gets acutely sick from SARS-CoV-2 develops the chronic form. Besides avoidance, what are your options for preventing Long COVID?
A 2023 study found that vaccination reduced the incidence of PCC (Post-COVID-19 condition), the medical term for Long COVID, from 1.4 percent to 0.4 percent. A Brazilian study found that vaccine boosters make a significant difference in preventing Long COVID. But vaccination doesn’t reduce the risk to zero. And not everyone is confident in vaccine safety.
Long VAX Syndrome
Perhaps more common than documented, postvaccination symptoms are real and, for some, last a long time. A 2024 survey found that for those who had previous acute COVID and developed Long COVID, getting vaccinated prolonged their Long COVID symptoms for more than one year. This combination of infection and vaccination suggests that Long COVID may be immunological rather than reactivation from viral reservoirs.
Many also develop postural orthostatic tachycardia syndrome (POTS) when their heart rate goes up dramatically when going from lying or sitting to standing. Symptoms include weakness, severe dizziness, and sometimes fainting. Some of these patients get better on their own after several months. Others respond to intravenous immunoglobulin. And some respond to taking oral steroids. Though the number of Long VAX cases with POTS is far fewer than for those with Long COVID, it’s a problematic condition for those patients.
Support Your Viral Immunity
It’s clear that you won’t get infected if you don’t get exposed to the virus. If you don’t get infected, you won’t get sick. However, that’s not possible for everyone. Another way to prevent severe viral infection is to support your viral immunity.
In my book Viral Immunity, I define viral immunity as the ability of the immune system to prevent, defend against, neutralize, and eliminate viruses from the body.
As I was in 2002 when the book was released, I am even more convinced now that viral infections are this century’s most important health issue. Prevention is the key to managing this tsunami of viral diseases.
3 Ways to Prevent Long COVID:
- Avoid acute infection.
- Get vaccinated.
- Improve your viral immunity.
Determinants for Getting Long COVID
In addition to the weaker immune status of modern people, other determinants, like age, matter. According to a 2023 CDC report, the prevalence of Long COVID range is about 7.5% of adults in the U.S. But those in the 40-54 age group are the most likely to experience Long COVID. And those over 55 years had the highest rate of severe Long COVID.
So does gender. Women are twice as likely to get Long COVID than men. Similarly, ME/CFS affects twice the number of women than men. Researchers look for a hormone connection. But women as family caretakers may have more run-down immunity or more exposure, so they are more susceptible to everyday viruses like EBV that are associated with both ME/CFS and Long COVID.
Other predictors of Long COVID risk include lower household income, being divorced or separated, being Hispanic, being gay or bisexual, and being female, according to a study posted on FIERCE Healthcare in 2023.
We Can Do Better
We need to do better. And we can do better.
First, improve your understanding of viruses and how they make us sick. Researchers found that even mild COVID infection causes T-cell exhaustion. T-cells are a type of white blood cell called lymphocytes that play a pivotal role in adaptive immunity. They prevent infection by fighting off viruses and defending against cancer and our response to allergens. They are produced in the bone marrow and mature in the thymus gland, therefore the designation “T” cell.
A 2026 paper describes how vitamins A, D, and C support T-cell immunity. Vitamin D is one of the most common nutrient deficiencies. I test every new patient for their Vitamin D status. According to a 2021 paper, zinc may target T-cell metabolism. Take enough vitamins A, D3, C, and zinc as foundation viral immunity supplements to support T-cells.
We can communicate public health matters better. Healthcare providers can contact all Long COVID cases, including the most vulnerable and economically impacted. Effective treatments need to be cost-effective. Since conventional health care failed ME/CFS patients and is failing to treat or manage Long COVID successfully, patients are on their own. We can listen to our patients better.
“Long-haulers saw and predicted the rise of long Covid before credentialed academics did.”
I am the author of two books on viruses, Beating the Flu and Viral Immunity, and a clinician who routinely treats ME/CFS patients; I predicted the rise of a chronic form of the SARS coronavirus early in the first year of the COVID-19 Pandemic. I also suspected we’d have a chronic form of SARS and MERS from the original outbreaks. But we didn’t see many chronic cases then because those infections were more aggressive with a higher fatality rate. More died from acute disease, thereby reducing the potential pool of chronic infection cases.
One of the most significant reasons for runaway chronic viral illness is that conventional doctors don’t understand it or know what to do about it. Patients get ignored. Long COVID confirmed what I already knew about ME/CFS: doctors can learn more by listening to patients than by reading medical journals. I learn both ways but always take extra time to hear a new patient’s story.
I’m not alone in this opinion. In “Surviving but Not Recovering,” Ed Young, a science writer for The Atlantic and The New York Times, wrote about how this complex condition defies modern medicine. Early in the COVID-19 Pandemic, his voice was both wise and compassionate. He humbly wrote that he learned more from interviewing patients than talking with their doctors.
“Long Covid taught me to seek expertise from actual patient experience, instead of from professional credentials.”
In a 2024 Time article, The Relentless Cost of Chronic Diseases, Alissa Quart relates that it took six months for her doctors to conclude that she had Long COVID. They told her that fainting spells and episodes of severe pain were caused by any number of reasons, as well as psychological conditions. Postural orthostatic tachycardia syndrome (POTS) was a likely reason.
She wrote that Long COVID can teach us to prioritize patient-centered care. This concept is not new to me or other functional medicine providers. Every day, I see individual variations of chronic illness – indeed, not all Long COVID patients are the same. We need better patient-centered care for this type of complex, chronic illness. A functional medicine model emphasizing restoring immune integrity is the key.
3 Things That Long COVID Is Not
- Long COVID is not a psychological condition. All chronic conditions have emotional overlaps, but that doesn’t mean what you’re experiencing is all in “your head.” Many experience different degrees of post-pandemic anxiety and depression, which can accompany Long COVID or occur without the pattern of somatic symptoms associated with Long COVID. Emotional issues are a symptom of the condition, not the cause.
- Long COVID is not an acute, temporary infection. It’s a long-term condition that occurs when a virus persists in the blood or tissue after acute infection or vaccination or disrupts immune function in a way that allows persistent symptoms. It can last years or longer.
- Long COVID is not only in the respiratory tract. It is a standard general term for a whole-body illness that persists after exposure to SARS-CoV-2 infection.
Questions To Ask If You Have Long COVID
- Have I been diagnosed accurately?
- Have I been treated effectively?
- Do I have any side effects from treatments?
- Do I still have at least three of the five most common symptoms of Long COVID?
- Where can I get the best care? Does my health insurance cover treatment?
Long COVID is not a medical term. The clinical term is post-acute sequelae of SARS-CoV-2 infection (PASC). The ICD code is U09.9. Using code U09.9 provides insight into diagnostics and treatments used by providers for patients presenting with Long COVID, for which treatment guidelines remain under development. It also helps with health insurance coverage and unemployment benefits. Other codes for specific symptoms, such as fatigue, cough, muscle aches, and headache, are also used.
5 Most Common Symptoms of Long COVID:
Post-exertional malaise
Cognitive impairment (“brain fog”)
Chest discomfort with or without an irregular heartbeat
Shortness of breath
What Should You Include in a Long COVID Supplement Stack?
In this chapter and previous chapters, I discussed many supplements for prevention and the early infection treatment of Long COVID. Here is a summary of the evidence-based supplements I use for patients in my practice and online followers.
| SUPPLEMENT | DAILY DOSAGE | WITH OR WITHOUT FOOD |
| Vitamin A | 10,000 IU | With |
| Vitamin C | 3,000-6,000 mg | Without |
| Vitamin D3 | 5,000 IU | With |
| N-Acetylcysteine (NAC) | 600 mg twice daily | Without |
| Glutathione (reduced liposomal) | 200 mg twice daily | Without |
| Zinc picolinate | 15 mg twice daily | With or without |
| Selenomethionine | 200 mcg twice daily | With or without |
| Asian Ginseng (12% ginsenosides) | 250 mg twice daily | Without |
| PROBIOMED 50 | 1 capsule daily | With |
| Nicotinamide mononucleotide (NMN) | 200 mg (2 capsules) once daily | Without |
| MitoQ | 20 mg | Before meals or without |
| Tollo19/Tollovid | 900 mg (3 capsules) twice daily | With or without |
| ImmunoKinoko 750 | 1500 g (2 capsules) twice daily | Before meals or without |
| Protease 375K | 1-3 capsules twice daily | With |
An April 2024 report by the New York Academy of Sciences called Long COVID is a significant and urgent public health priority. That’s important, but is medical science a little too late with insufficient options to offer patients?

Comprehensive Workup & Active Management
The rates of Long COVID have dropped thanks to increased immunity from natural exposure and vaccination, milder variants, better safeguards, improved early treatment, and fewer cases. The current rate of Long COVID is 11 percent among the unvaccinated and 5 percent among those with two or more vaccine doses. That’s still too many suffering from Long COVID.
If you have symptoms, get a comprehensive workup with adequate diagnostic testing. Four biological mechanisms factor into the cause and persistence of Long COVID: (1) an ongoing viral reservoir, (2) immune dysregulation, (3) reactivation of a latent virus-like EBV, and (4) lasting tissue damage and dysfunction from the initial acute infection.
Take Long COVID seriously. If your doctor doesn’t take your symptoms seriously, go somewhere else.
At our integrative medical center, after a thorough workup and examination, we test for all these parameters. Then, we outline the best treatments for each patient.
Menu of Services for Long COVID at DaSilva Institute:
- Comprehensive laboratory and advanced testing for viral antibodies, immune cell populations, and gut microbiome integrity
- Targeted professional-grade nutritional supplements and herbal extracts
- Acupuncture for vagal nerve regulation
- IV nutrient therapies, including high-dose vitamin C and electrolytes.
- EBOO apheresis
- SOT antisense therapy for Epstein-Barr reactivation
- Targeted professional-grade nutritional supplements and herbal extracts
- Prescription medications as needed
Antisense therapy (SOT) uses nucleic acid-based oligonucleotides and is widely used in treating cancer, viral or general infections, and genetic disorders. The mechanism of action is through RNA-mediated interference (RNAi), where short double-stranded RNA (dsRNA) molecules cause messenger RNA (mRNA) degradation. RNA interference is a physiological process required for the regulation of gene expression. We are pleased with the results from SOT.
Our goal for every patient we see is the resolution of chronic disease, a return to normal—a state without illness or residual symptoms, and the continuation of a healthy, happy, and productive life.
CONTACT INFORMATION
DaSilva Institute
3131 South Tamiami Trail Suite 202
Sarasota, Florida 34239
(941) 388 0940
Selected Citations
Ancona G, Alagna L, Alteri C, Palomba E, Tonizzo A, Pastena A, Muscatello A, Gori A, Bandera A. Gut and airway microbiota dysbiosis and their role in COVID-19 and long-COVID. Front Immunol. 2023 Mar 8;14:1080043. https://doi:10.3389/fimmu.2023.1080043. PMID: 36969243; PMCID: PMC10030519.
Apostolou, P., Iliopoulos, A., Beis, G., & Papasotiriou, I. (2022). Supportive Oligonucleotide Therapy (SOT) as a Potential Treatment for Viral Infections and Lyme Disease: Preliminary Results. Infectious Disease Reports, 14(6), 824-836. https://doi.org/10.3390/idr14060084
Asadi-Pooya AA, Nemati M, Shahisavandi M, Nemati H, Karimi A, Jafari A, Nasiri S, Mohammadi SS, Rahimian Z, Bayat H, Akbari A, Emami A, Eilami O. How does COVID-19 vaccination affect long-COVID symptoms? PLoS One. 2024 Feb 7;19(2):e0296680. doi: 10.1371/journal.pone.0296680. PMID: 38324547; PMCID: PMC10849259.
Davis, H. E., McCorkell, L., Vogel, J. M., & Topol, E. J. (2023). Long COVID: Major findings, mechanisms and recommendations. Nature Reviews Microbiology, 21(3), 133-146. https://doi.org/10.1038/s41579-022-00846-2
Durstenfeld, M. S., Weiman, S., Holtzman, M., Blish, C., Pretorius, R., & Deeks, S. G. Long COVID and post-acute sequelae of SARS-CoV-2 pathogenesis and treatment: A Keystone Symposia report. Annals of the New York Academy of Sciences. https://doi.org/10.1111/nyas.15132
Fatima, S., Ismail, M., Ejaz, T., Shah, Z., Fatima, S., Shahzaib, M., & Jafri, H. M. (2023). Association between long COVID and vaccination: A 12-month follow-up study in a low- to middle-income country. PLOS ONE, 18(11). https://doi.org/10.1371/journal.pone.0294780
Jin H, Lu L, Fan H. Global Trends and Research Hotspots in Long COVID: A Bibliometric Analysis. International Journal of Environmental Research and Public Health. 2022 Mar;19(6):3742. http://doi.org/10.3390/ijerph19063742.
Imbalzano E. Natural Course of COVID-19 and Independent Predictors of Mortality. Biomedicines. 2023 Mar 17;11(3):939. https://doi:10.3390/biomedicines11030939. PMID: 36979918; PMCID: PMC10046319.
Komaroff, A. L., & Lipkin, W. I. (2023). ME/CFS and Long COVID share similar symptoms and biological abnormalities: Road map to the literature. Frontiers in Medicine, 10, 1187163. https://doi.org/10.3389/fmed.2023.1187163
Kouchek, M., Aghakhani, K., & Memarian, A. (2024). Demographic study of patients’ mortality rate before and after the COVID‐19 outbreak: A cross‐sectional study. Health Science Reports, 7(2). https://doi.org/10.1002/hsr2.1845
Lundberg-Morris L, Leach S, Xu Y, Martikainen J, Santosa A, Gissln M et al. Covid-19 vaccine effectiveness against post-covid-19 condition among 589 722 individuals in Sweden: population based cohort study BMJ 2023; https://doi.org/383:e076990
Marra AR, Kobayashi T, Callado GY, et al. The effectiveness of COVID-19 vaccine in preventing post-COVID conditions: a systematic literature review and meta-analysis of the latest research. Antimicrobial Stewardship & Healthcare Epidemiology. 2023; https://doi:10.1017/ash.2023.447
Michael Hollifield, Karen Cocozza, Teresa Calloway, Jennifer Lai, Brianna Caicedo, Kala Carrick, Ruth Alpert, and An-Fu Hsiao.Improvement in Long-COVID Symptoms Using Acupuncture: A Case Study.Medical Acupuncture.Jun 2022.172-176. http://doi.org/10.1089/acu.2021.0088
Orlando L, Bagnato G, Ioppolo C, Franzè MS, Perticone M, Versace AG, Sciacqua A, Russo V, Cicero AFG, De Gaetano A, Dattilo G, Fogacci F, Tringali MC, Di Micco P, Squadrito G, Imbalzano E. Natural Course of COVID-19 and Independent Predictors of Mortality. Biomedicines. 2023 Mar 17;11(3):939. https://doi:10.3390/biomedicines11030939. PMID: 36979918; PMCID: PMC10046319.
Pfaff, E. R., Madlock-Brown, C., Baratta, J. M., Bhatia, A., Davis, H., Girvin, A., Hill, E., Kelly, L., Kostka, K., Loomba, J., McMurry, J. A., Wong, R., Bennett, T. D., Moffitt, R., Chute, C. G., Haendel, M., Consortium, C., & Consortium, T. R. Coding Long COVID: Characterizing a new disease through an ICD-10 lens. MedRxiv. https://doi.org/10.1101/2022.04.18.22273968
Sergi, C. M. (2022). The Role of Zinc in the T-Cell Metabolism in Infection Requires Further Investigation – An Opinion. Frontiers in Immunology, 13. https://doi.org/10.3389/fimmu.2022.865504
Tanno, L. K., Casale, T., & Demoly, P. (2020). Coronavirus Disease (COVID)-19: World Health Organization Definitions and Coding to Support the Allergy Community and Health Professionals. The Journal of Allergy and Clinical Immunology. in Practice, 8(7), 2144-2148. https://doi.org/10.1016/j.jaip.2020.05.002