
Empowering Patients with Long COVID
For doctors and healthcare providers
Rebecca didn’t feel well. It was six months since her acute COVID infection. She hadn’t been admitted to the hospital with her initial infection and never used a ventilator. However, she had fatigue and malaise severe enough to keep her in bed for two weeks after the acute phase. Then, a slow recovery followed over a few months, but she wasn’t back to her normal, vibrant self.
Though she was no longer acutely sick and didn’t need to stay in bed, she still felt unwell. She had a cluster of vague symptoms, including memory lapses and tiredness that didn’t improve with rest. She was often light-headed and had fainting spells. Sometimes, her heart raced like it wanted to jump out of her chest. She didn’t have a fever but often felt warm, even in her air-conditioned home. She checked her temperature several times daily. It was usually normal, but sometimes it was 99.5 to 100 degrees. Her primary care doctor called it an intermittent low-grade fever and not a concern.
Does she have Long COVID or an extended recovery? Or some other condition? Would additional lab tests be useful? Does she need a chest X-ray? An electrocardiogram? Or a brain MRI? The COVID-19 Pandemic makes these common, seemingly inconsequential clinical questions important.
As a starting point, to determine if your patient has had COVID, test their Anti-SARS-CoV-2 Spike Protein IgG antibody level. A positive result confirms past infection or vaccination. But persistent, higher levels are also associated with Long COVID.
General questions to ask include: how severe was her initial acute illness? Was she hospitalized? These clinically useful facts were likely documented in her medical chart. Review past lab test results and doctors’ notes from previous visits. In your opinion, were her workups complete?
Since 2020, many have had multiple SARS-CoV-2 infections. It is not uncommon for the first infection to be mild; the second or third one becomes more severe, sometimes lasting a month or longer. Your patient starts to get better, but recovery stalls. The more times you get COVID, the greater your chance of developing Long COVID. It settles in like a cloudy sky with rainy days that never clear.
Rebecca is a fictitious composite case but with symptoms all too common among Long COVID patients.
Diagnosing Long COVID
Like ME/CFS, Long COVID is a medical enigma. There is no laboratory test for either condition; chest X-rays or electrocardiograms are usually normal.
Both conditions are syndromes. The National Institutes of Health (NIH) defines a syndrome as a recognizable complex of symptoms and physical findings that indicate a specific condition for which a direct cause is not necessarily understood.
Once medical science identifies a causative agent, like a virus or a process like cancer, with a degree of certainty, physicians refer to the presentation as a disease, not a syndrome. Traditional healthcare providers are trained to diagnose diseases with a known cause, like acute COVID caused by the SARS-CoV-2 virus. It’s an infectious disease with an ICD-10 Diagnostic Code U07.1. The code for the post-acute sequela of COVID-19 is U09.9.
It’s still unclear what causes Long COVID. Though it occurs after acute SARS-CoV-2, Long COVID patients are not carriers of live coronaviruses and can’t infect someone else. Some studies found reservoirs of viral activity sequestered in the tissues of Long COVID patients but are not considered infectious. Some cases occur after COVID vaccination. My own case was after my second COVID shot.
However, even with the uncertainty of chronic viral disease, clinicians can help Long COVID patients improve their quality of life and eventually beat Long COVID. It’s a high bar to achieve, but it’s a challenge clinicians need to accept.

Symptoms of Long COVID
The most common symptoms of Long COVID are fatigue without having done anything, post-exertional fatigue, and brain fog. However, many additional symptoms occur, though not in all patients and not at the same time.
General symptoms
- Extreme tiredness or fatigue that interferes with daily life.
- Symptoms that get worse after physical or mental effort (also known as “post-exertional malaise”)
- Low-grade fever or fever-like warmth sensation
Neurological symptoms
- Difficulty thinking or concentrating (“brain fog”)
- Headache, typically low-grade but persistent
- Sleep difficulty, unrefreshed rest.
- Dizziness when you stand up (lightheadedness)
- Pins-and-needles sensation in the hands and feet
- Change in smell or taste.
- Depression or anxiety
Respiratory and heart symptoms
- Difficulty breathing or shortness of breath.
- Cough
- Chest pain
- Fast-beating or pounding heart and heart palpitations (irregular heart rate)
Digestive symptoms
- Diarrhea
- Stomach pain.
- Abdominal bloating
Other symptoms
- Joint or muscle pain
- Rash
- Changes in the menstrual cycle
- Mood changes, depression
Laboratory Tests for Long COVID
There is no specific lab test that clinically defines Long COVID. However, some useful tests and profiles emerged during the 2019 Pandemic. These are some of the tests I order on the first visit for patients who I suspect have Long COVID. You may order different tests, including markers for autoimmunity like ANA or anti-dsDNA. However, among my Long COVID patient population very few have autoimmune conditions, so I typically don’t order these studies on the first visit.
Hormone deficiencies can exaggerate Long COVID symptoms. Consider adding total testosterone for men and women, and estradiol and progesterone for women.
| COMPREHENSIVE LONG COVID PANEL | Quest | Labcorp |
| Complete Blood Count (CBC) with differential | 6399 | 005009 |
| Comprehensive Metabolic Profile (CMP 14) | 1031 | 322000 |
| Cortisol, Total | 367 | 004051 |
| C-Reactive Protein, highly sensitive (CRP-hs) | 10124 | 120766 |
| CD4:CD8 Ratio Profile | None | 505271 |
| DHEA-Sulfate | 402 | 004020 |
| D-Dimer, Quantitative | 8659 | 115188 |
| Erythrocyte Sedimentation Rate (ESR) | 809 | 005215 |
| Ferritin | 457 | 004598 |
| Fibrinogen Activity | 461 | 001610 |
| Immunoglobulin G (IgG), Subclasses 1-4 | 7903 | 209601 |
| Immunoglobulin M (IgM) | 545 | 001792 |
| SARS-CoV-2 Antibody (IgG), Spike, Quantitative | 34499 | 164090 |
| T- and B-Lymphocyte Profile | 39588 | 096917 |
| Vascular Endothelial Growth Factor (VEGF) | 14512 | 117021 |
| Vitamin D, 25-hydroxy | 17306 | 081950 |
| Interleukin 6 (IL-6) |
Even though there’s no definitive lab marker for Long COVID, I’ve found that if six of these lab markers are positive, they had a positive antigen rapid home test or a positive PCR at the time of the original infection, and my patient has a cluster of the main systems, and a very high SARS-CoV-2 IgG, Spike, antibody titer, it’s clinically safe to assume the patient has Long COVID.
Now comes the hard part. You’ll have to tell your patient that you suspect Long COVID.
When Working with Long COVID Patients:
- Never dismiss them as being unable to get better.
- Don’t minimize their efforts, no matter how small or feeble.
- Support their attempt to improve in all ways you can, medical and non-medical.
- Be patient if they are slow in achieving results.
- If their progress falters, encourage them to try again, not to give up, and to renew their efforts.
- Sometimes, they need to take a break from trying to improve.
- Be okay if they need extra rest or require more help.
- Train your staff to deal compassionately but effectively with the cognitive impairment associated with Long COVID.
Common Questions Long COVID Patients May Ask:
What’s the Difference Between Long COVID and ME/CFS?
The symptoms are similar. But the cause and history are different. Long COVID is a consequence of the COVID-19 Pandemic, a post-acute condition defined by symptoms that started after January 2020.
What’s the Difference Between Long COVID and POTS?
Postural Orthostatic Tachycardia Syndrome is defined as a change in blood pressure that drops from lying or sitting to standing. Long COVID patients may also have POTS.
Do Long COVID Cases Have Persistent SARS-CoV-2 Viral Reservoirs?
We don’t know, but researchers published a 2024 report in the Lancet describing their finding that Long COVID patients may have persistent viral infection as long as fourteen months.

Resources For Healthcare Providers
To truly understand what’s happening with Long COVID patients, a wiring diagram, a surface map of viral immunity, is not enough. A flow chart is not enough to contain the complexity of this viral condition. It’s not as easy as connecting the dots. It’s more like a network, a promiscuous one, with more connections than we’d assume. How can we define an organized, easily understandable cause followed by a single course of treatment in such a fuzzy network?
Nothing in Long COVID is precisely delineated. And there’s likely not one network, but many. Biological life has its rules, but we don’t understand most. But that shouldn’t discourage you from working with Long COVID patients.
Here are some online services for healthcare providers:
- CDC Post-COVID Conditions: Information for Healthcare Providers
- AAPM&R (American Academy of Physical Medicine and Rehabilitation): Long COVID (PASC) Resources
- NIH Long COVID
- John Hopkins Medicine: COVID-19 Rehabilitation Resources
Support for Long COVID Patients
Your patients need to know they’re not alone. Long COVID occurs worldwide. A 2023 Lancet article reports at least 65 million people have symptoms after COVID infection.
Make a list of local and online support groups, add a page to your office website, or start your own. Encourage your patients to participate in a support group. There’s comfort in a shared understanding of a difficult-to-grasp condition. However, group meetings are only for some. Many prefer the one-on-one traditional doctor-patient relationship.
Should you start a support group? In-person, one evening per week, or once a month? Or a video chat group online? Sharing your latest insights, conferences you attended, and articles you read during monthly Zoom meetings inspires confidence in your work and establishes professionalism. It shows patients you care about them.
Online Support Groups:
- Patient-Led Research and Collaboratives: The Patient-Led Research Collaborative is a group of Long COVID patients, and those with associated illnesses such as ME/CFS and POTS, who are also researchers.
- Long COVID Association: The LONG COVID ASSOCIATION was established to reduce the suffering of Long COVID patients. They connect scientists, researchers, the medical community, patients, and caregivers with scientific information, resources, and medical providers for the benefit and the health of Long COVID patients and the community.
- PandemicPatients.org: Pandemic Patients is a 501(c)(3) non-profit organization that works to relieve the harm caused by COVID-19 and Post-COVID Conditions. During the coronavirus pandemic, Christopher Floyd and Andrew Wylam founded the organization on May 26, 2021. The founders launched Pandemic Patients intending to provide support and services to those affected by COVID-19.
Long COVID on Social Media
Do you participate on social media? It’s another way to inform your patients about your reading, the conferences you attended, and the extra courses you took. Let them know your experience, for example, what supplements work or don’t help.
- Twitter (now X) – Long Covid Support
- Facebook – LONG COVID ASSOCATION
- Instagram – Long Covid Support
The National Institutes of Health (NIH) provides a Long COVID Social Media Toolkit with downloadable information cards you can repost to your social media sites.
Website Communication
Do you have time to write blogs about Long COVID to post on your website? Anecdotal patient stories are often better received than technical, impersonal, detailed writeups. Reserve those for case studies in clinical journals.
Do you email a weekly or monthly newsletter? Let your patients know if you’re participating in a study. Tell them if you have a new treatment or therapy. Keeping your patients informed boosts confidence in your work and helps them stay connected.
Are Cognitive Therapies Helpful?
The rarity of complete recovery in Long COVID patients who attend conventional treatment centers informs us that traditional biomedicine doesn’t know what causes it or how to treat it effectively and safely.
For example, brain retraining for cognitive dysfunction and wakefulness drugs for drowsiness and fatigue, common first choices for Long COVID treatment, do not address the underlying immunological and metabolic changes at the root of Long COVID. Though some patients experience minor benefits, they are ineffective in providing lasting recovery because it is a post-viral condition, not a stress-induced disorder.
Cognitive behavioral therapy (CBT), a widely used “talk therapy,” may help some navigate the psychological journey of Long COVID. Still, CBT does not resolve somatic factors like chronic pain associated with low-grade inflammation. And it does nothing to rebalance hormones or address mitochondrial dysfunction.
Based on my clinical experience, I’ve concluded that addressing biochemical, metabolic, and immunological imbalances is the most beneficial approach, followed by psychological counseling and cognitive therapies.
I understand that some Long COVID patients may have post-traumatic stress syndrome induced by the ordeal of being in a hospital ICU for a few weeks or longer. In these cases, CBT may have been beneficial and can be used to parallel treatments that address biological causes.
Though CBT has a place in a comprehensive approach to managing Long COVID, deeper-acting biological therapies are the primary approaches to resolving this condition. Remember, Long COVID is not a psychological condition. However, patients have emotional and cognitive issues.
Before starting any form of cognitive therapy or psychological counseling, get my recommended panel of blood tests. For example, if cortisol and DHEA levels are too low or above the upper end of the reference range, talk therapy will have limited or no benefit. First address adrenal hormone imbalances. Then, start CBT or other psychological therapies.
Physical Therapy and Body Movement Practices
Body movement practices like physical therapy, tai qi, and therapeutic yoga can improve motor function, stabilize balance, lessen joint and muscle pain, and lift mood and energy. Although useful, these activities are not biological answers to the immunological needs of Long COVID patients.
Combining therapies may provide more relief. For example, yoga and deep breathing can be combined with TENS, or red-light exposure could follow a yoga practice.
Referring Patients to Long COVID Treatment Centers
You can only do so much for the more severe cases and most needy patients. When you need help, do you have a trusted referral? The advantage of a larger treatment center is greater experience with more patients, access to university databases, and they have the funding to offer therapies that a small practice can’t afford.
Here are three that meet my standards. DaSilva Institute is the group I work with in Sarasota, Florida.
In Sarasota, I refer to Hyperbaric Centers of Southwest Florida. This group is well-experienced with the medical use of hyperbaric oxygen therapy, including for Long COVID. Another is Aviv, a specialized hyperbaric clinic that uses the medical program developed by Dr. Shai Efrati, Director of the Sagol Center for Hyperbaric Medicine and Research at the Shamir Medical Center in Israel. However, hyperbaric oxygen therapy is more common now, with local options available in most large cities.
John Hopkins Post-Acute COVID-19 Team (JH PACT) Program is a collaboration between the Division of Pulmonary & Critical Care Medicine and the Department of Physical Medicine and Rehabilitation. Their goal is to provide interdisciplinary, standardized care to address the unique needs of COVID-19 survivors.
“Long COVID has put a spotlight on the seriousness of infection-triggered complex multisystem chronic illness.”
John Hopkins Medicine Lyme Disease Research Center
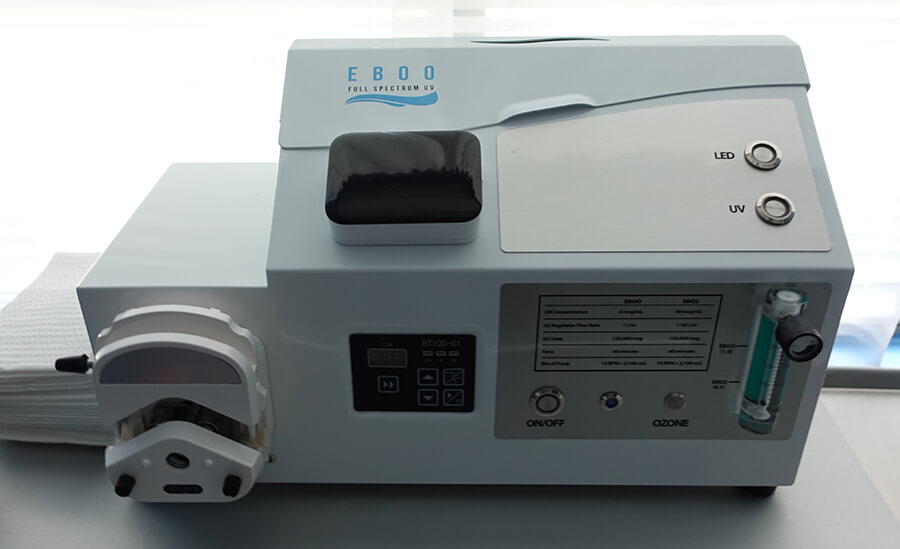
Winter 2024 Newsletter DaSilva Institute provides comprehensive care for chronic medical conditions including Long COVID. Treatment options include ultraviolet blood irradiation, advanced Extracorporeal Blood Oxygenation and Ozonation (EBOO) apheresis, intravenous nutritional infusions, acupuncture, hormone therapies, and naturopathic medicine.

DaSilva Institute
3131 South Tamiami Trail Suite 202
Sarasota, Florida 34239
(941) 388 0940
Chapter Summary
Long COVID is complicated. Like other chronic conditions and intractable diseases, it is difficult for patients and their doctors. Some improve but don’t get better. Their recovery stalls, plateaus, and becomes clinically entrenched. They present with the same complaints and symptoms, week after week, month after month. It’s exhausting. I know. But be patient with your patients. They want to get better, feel well again, and have enough energy to get through their day like everyone else.
Selected Citations
Calvo, F., Karras, B. T., Phillips, R., Kimball, A. M., & Wolf, F. (2003). Diagnoses, Syndromes, and Diseases: A Knowledge Representation Problem. AMIA Annual Symposium Proceedings, 2003, 802. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1480257/
Davis, H. E., McCorkell, L., Vogel, J. M., & Topol, E. J. (2023). Long COVID: Major findings, mechanisms and recommendations. Nature Reviews Microbiology, 21(3), 133-146. https://doi.org/10.1038/s41579-022-00846-2
Di Paolo N, Bocci V, Salvo DP, et al. Extracorporeal Blood Oxygenation and Ozonation (EBOO): A Controlled Trial in Patients with Peripheral Artery Disease. The International Journal of Artificial Organs. 2005;28(10):1039-1050. https://doi:10.1177/039139880502801012
Jin, H., Lu, L., & Fan, H. (2022). Global Trends and Research Hotspots in Long COVID: A Bibliometric Analysis. International Journal of Environmental Research and Public Health, 19(6). https://doi.org/10.3390/ijerph19063742
Koc HC, Xiao J, Liu W, Li Y, Chen G. Long COVID and its Management. Int J Biol Sci. 2022 Jul 11;18(12):4768-4780. https://doi:10.7150/ijbs.75056.
Lin K, Tung C. The Regulation of the Practice of Acupuncture by Physicians in the United States. Med Acupunct. 2017 Jun 1;29(3):121-127. https://doi:10.1089/acu.2017.1235. PMID: 28736588; PMCID: PMC5512332.
McCorkell L, S Assaf G, E Davis H, Wei H, Akrami A. Patient-Led Research Collaborative: embedding patients in the Long COVID narrative. Pain Rep. 2021 Apr 13;6(1): e913. https://doi.org:10.1097/PR9.0000000000000913.
Trager RJ, Brewka EC, Kaiser CM, Patterson AJ, Dusek JA. Acupuncture in Multidisciplinary Treatment for Post-COVID-19 Syndrome. Med Acupunct. 2022 Jun 1;34(3):177-183. https://doi:10.1089/acu.2021.0086. Epub 2022 Jun 16. PMID: 35821795; PMCID: PMC9248328.
Umesh, A., Pranay, K., Pandey, R. C., & Gupta, M. K. (2022). Evidence mapping and review of long-COVID and its underlying pathophysiological mechanism. Infection, 50(5), 1053-1066. https://doi.org/10.1007/s15010-022-01835-6