We’re Getting It All Wrong About Long COVID
| | Reading Time: 6 minutes
Though we’re in the waning stage of more than three years into the pandemic, “long COVID” retains the stigma of a mystery disease. But is it a mystery? Or an ambiguous, complex syndrome not uncommon in other post-infectious conditions?
Long COVID is not an unexpected mystery disease—many other infections cause similar symptoms. Don’t be misinformed and scared by popular media pieces that stigmatize Long COVID patients as either an overly complex condition that defies science and medicine or blames patients for imaging symptoms.
In a Vox article by Dylan Scott, the author states that imminent scientists agree there is no single cause of long COVID. That’s not technically true because SARS-CoV-2 is the causative viral infection and the source of many symptoms, much like other post-viral illnesses. Unfortunately for patients, wrong thinking plays into the outdated paradigm of “one cause, one cure” driven by pharmaceutical companies because of the high profit for targeted drugs. It presents a hopeless scenario to all long COVID patients when, in fact, there is a good possibility that most can recover.
What is post-acute infectious syndrome?
SARS-CoV-2 is not unique in triggering post-acute chronic symptoms. Post-acute infectious syndrome (PAIS) occurs in some individuals after infection by viruses, bacteria, or spirochetes like Lyme disease. At least ten unexplained PAISs are associated with a documented viral infection, including SARS-CoV-2, SARS, Ebola, Polio, Chikungunya, Epstein-Bar Virus, and Dengue. [Choutka 2022]
Post-dengue fatigue syndrome (PDFS) includes symptoms of fatigue, muscle weakness, and neurological complaints [Umakanth], like long COVID. Symptoms start abruptly with severe headaches, pain behind the eyes, muscle aches, loss of appetite, and fever. Like SARS-CoV-2, the spectrum of symptom severity ranges from mild to life-threatening from Dengue shock syndrome. Dengue can infect many organs, including the liver, brain, heart, and intestines. Common PDFS symptoms include malaise, severe persistent fatigue worse after exertion, impaired memory, poor concentration (“brain fog”), joint pain, and additional non-specific symptoms. PDFS can last months or become chronic. These symptoms sound much like Long COVID because they have common pathways in the body.
I know what it’s like because I experienced extreme fatigue, weakness, and brain fog after a near-fatal attack of Dengue Fever during one of my research trips to the upper Peruvian Amazon. I could barely tie my shoes without getting exhausted. And, I also had autoimmune reactions, including swollen joints. My knees were so swollen; I couldn’t fit into my pant legs! I wore baggy pants to work and shorts at home.
In my case, I saw the best doctors in San Diego, including at Scripps Clinic. Some were colleagues and friends. All were kind and professional but useless when offering me any help. As in my case, most long COVID patients suffer on their own.
Some patients, like I was, are more proactive, like the health and fitness guru Oz Garcia. He hits the mark in his recent book, After Covid: Optimize Your Health in a Changing World. His natural health recommendations will help many recover from acute and post-COVID. They will likely help many others prevent Long COVID. However, recovering from long COVID is complicated.
Similar post-infectious symptoms occurred after the original SARS epidemics. SARS-CoV-1 emerged in 2003 from Foshan, Guangdong region in China, next to Hong Kong. Another coronavirus, MERS, emerged in Saudi Arabian in 2012. Both had a higher death rate than SARS-CoV-2 and more severe acute illness. Follow-up studies found that close to 50 percent of survivors had chronic fatigue up to a year after recovery from the acute phase. [O’Sullivan 2021]
PAISs, including Long COVID, are characterized by a failure of the body’s ability to recover fully from acute infection. Like with Long COVID, the pathogen is undetectable by standard laboratory methods. I’ll write about these tests in a separate blog.
Body system pathways that lead to Long COVID
One of the best papers I’ve read on Long COVID [Davis 2023] is a review article published in Nature Reviews Microbiology. The authors suggest a pathway of body systems most likely to become part of a patient’s long COVID presentation. This biological map is consistent with my understanding of viral infections, as I wrote in Viral Immunity and Beating the Flu, a book on the H5NI pandemic avian influenza, the “bird flu.”
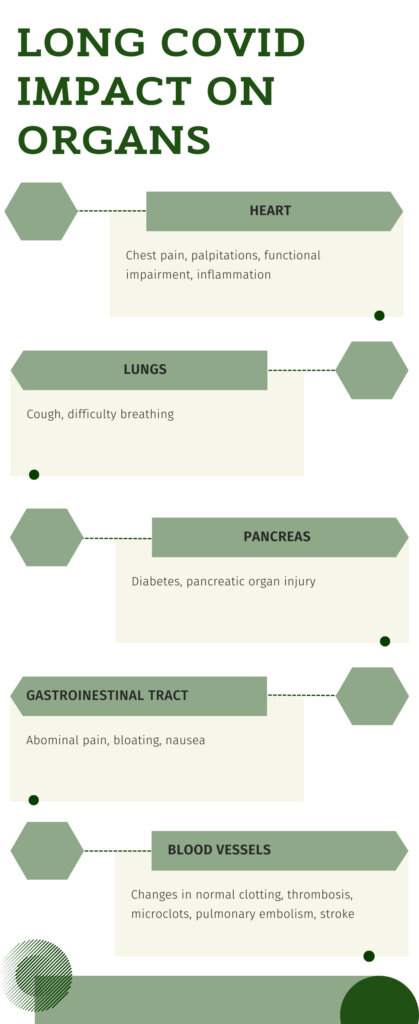
Long COVID is a multisystem condition with more than 200 symptoms beyond the respiratory tract. Symptoms of long COVID include profound unrelenting fatigue and weakness, irregular heart rate, numbness of the extremities, and malfunction of the liver or bladder.
After initial infection, the body’s immune system either clears the virus, and you get better, or the virus bypasses some of the immune barriers and goes deeper into tissues and cells. When non-specific immune imbalances occur, reactivation of dormant herpes viruses like Epstein-Barr virus (HIV-4) and HIV-6 can cause symptoms of PAISs.
Diarrhea and other gastrointestinal symptoms are common in these cases due to the impact of SARS-CoV-2 on the gut microbiome. SARS-CoV-2 induced dysbiosis can cause many of the symptoms associated with Long COVID.
Virally infected tissue triggers an autoimmune response, not to the virus but to the tissue where the virus harbors, like the joints or blood vessels. Clotting along with endothelial changes can occur, causing spontaneous bruising. And neurological impairment is caused by dysfunctional nerve signaling in the brain stem and vagus nerve, causing chronic fatigue and Postural tachycardia syndrome (PoTS).
These symptoms make sense because dysregulation of these five body systems can cause all the symptoms linked to Long COVID. The same applies to symptoms related to ME/CFS and Dysautonomia.
The pandemic will end, but Long COVID will not go away
Long COVID differs from post-COVID when recovery gets delayed for 2-4 weeks. Slow healing is typical for severe respiratory viral infections in less healthy people. But Long COVID is different. It’s a syndrome, a cluster of symptoms that varies from patient to patient and persists for years.
Once it becomes persistent, Long-COVID clinically presents much like myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) or a type of dysautonomia called postural orthostatic tachycardia syndrome (PoTS). According to The Dysautonomia Project, dysautonomia is an umbrella term for autonomic nervous system disorders.
Researchers report that at least 10-20 percent of those infected with COVID-19 develop long COVID. The most common age group is between 36 and 50 years. In comparison, the worst outcomes for acute COVID-19 are in those over 50 years. The occurrence of long COVID is highest in hospitalized cases: 50-70% versus 10-30% of patients who weren’t in the hospital.
But children can experience long COVID too. A 2022 systematic review paper found that about 25% of children and adolescents with acute COVID-19 developed chronic fatigue and mood and sleep changes consistent with long COVID.
What are your chances of getting better if you have Long COVID?
Most conventional doctors are unfamiliar with treating ME/CFS and the conditions associated with dysautonomia. They prescribe drugs to treat symptoms that don’t address the underlying complexity of these conditions. So, it’s not surprising that no specific, effective treatments for ME/CFS or PoTS exist. The average clinician expects Long COVID patients will suffer the same fate. But is that all there is to it?
I’ve treated ME/CFS and POTS patients over many decades. And at our integrative medical center, we successfully treat chronic Lyme disease patients. The majority improve, and many get better as their condition gradually goes into remission. I know it’s oversimplifying to equate long COVID with ME/CFS. But there are similarities, and both are without a specific cure, but that doesn’t mean they can’t be safely and effectively treated.
Decades ago, as an enthusiastic young clinician, I assumed that positive energy and suitable treatments with good medicine were adequate. But that approach only worked some of the time. I discussed my dilemma with my mentor, Sheldon Hendler, an accomplished trumpet player who once jammed with the Buena Vista Social Club and had a double Ph.D. (in biochemistry and virology) plus an M.D.
He listened attentively and sincerely. Then, he said: “For every complex, difficult-to-treat condition, there’s a simple cure…that doesn’t work.”
After forty years of clinical practice, I can attest to his wisdom: a simple, safe, and effective solution doesn’t exist for complex, multifaceted conditions like long COVID. But that doesn’t mean we don’t have ways to manage the effects of the illness or treatments that alter the course of the disease⎯bending the curve towards healing and complete recovery.
A wiser approach is needed.
__________________________
Selected References
Choutka, J., Jansari, V., Hornig, M. et al. Unexplained post-acute infection syndromes. Nat Med 28, 911–923 (2022). https://doi.org/10.1038/s41591-022-01810-6
Davis, H.E., McCorkell, L., Vogel, J.M. et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol 21, 133–146 (2023). https://doi.org/10.1038/s41579-022-00846-2
Lopez-Leon, S., Wegman-Ostrosky, T., Ayuzo del Valle, N.C. et al. Long-COVID in children and adolescents: a systematic review and meta-analyses. Sci Rep 12, 9950 (2022). https://doi.org/10.1038/s41598-022-13495-5
Oliver O’Sullivan. Long-term sequelae following previous coronavirus epidemics. Clinical Medicine Jan 2021, 21 (1) e68-e70; https://www.rcpjournals.org/content/clinmedicine/21/1/e68
Umakanth, M. (2018) Post Dengue Fatigue Syndrome (PDFS) among Dengue IgMAntibody Positive Patients at Batticaloa Teaching Hospital, Sri Lanka. Open Access Library Journal, 5: e4798. https://doi.org/10.4236/oalib.1104798
Our integrative medical center treats many patients with undiagnosed multisystem fatigue syndromes. Most have a history of microbial infection, including Lyme disease. And many have laboratory studies that reveal antibodies to previous infections, including Epstein-Barr Virus (EBV) and Human Herpes Viruses (HHV).