How to Lower Inflammation for Health and Longevity
| | Reading Time: 8 minutes
Medical researchers found that chronic diseases have a link to inflammation. However, the inflammation story is complicated. To take control of your health, the first step is to learn the laboratory tests that measure inflammation and the best ways to lower inflammation naturally.
A Case Study
She had MRSA, antibiotic-resistant Staphylococcus aureus, and other bacteria including Escherichia coli (E. coli), a bacterium that lives in the gut. But, people with low immunity or diabetes can get E. coli infection outside the intestinal tract. E. coli if often antibiotic resistant. She didn’t have diabetes or wasn’t immunodeficient. Where did Maryanne get these infections and why were both antibiotic resistant?
As it turned out, she traveled to the Caribbean for a medical procedure not available in the US. Though the top floor of the hospital was reserved for US patients, caregivers moved freely between the lower levels where doctors treated local patients and the private level where they managed Maryanne’s case. The infection found a way to the exclusive top floor, invaded her forehead and moved onto her scalp.
Under a hairpiece, the entire front left side of her scalp was red and irritated; her silver hair eroded exposing crusty, angry skin. A section of hair was gone, eaten away by the infection. The first course of antibiotics helped for a few weeks, but the bacterial infection returned. After additional courses of different antibiotics, her medical doctors said there was nothing more to do. She would lose her hair. It could get worse.
Treatment
I explained that her tissue terrain was out-of-balance and her immunity weakened. She needed immune support. I prescribed high dosages of beta-glucan, an immune-stimulating natural compound found in mushrooms and yeast. Boosted her vitamin C and zinc, also injected natural antimicrobials and compounds that support the extracellular matrix (ECM) to improve the skin microenvironment. The ECM is a network under the skin that interconnects with the lymphatic system and essential for wound healing and tissue repair. She took probiotics.
In the following weeks, the angry inflammation calmed. By the end of three months, new hair grew back. That was ten years ago. Maryanne’s skin and scalp remain free of infection.
What Is Inflammation and Why Does It Matter?
Acute inflammation is a normal reaction of the body to infection, tissue damage caused by injury, or irritants like a splinter in your finger. Acute inflammation is the body’s way of protecting and healing itself.
Symptoms & Signs of Acute Inflammation:
- Pain in the local area that is sore and sensitive when touched or moved.
- Swelling caused by a buildup of fluid.
- Redness caused by local capillaries filling with more blood.
- Heat because of more blood in the area.
- Immobility because of temporary loss of function in the inflamed area.
- Fever

However, persistent chronic inflammation is different. It may start as acute inflammation but can last for months or years. Or, it can begin silently. Unless you measure your markers, you wouldn’t know your body harbored inflammation. When activated, chronic inflammatory pathways might even trigger autoimmune diseases like rheumatoid arthritis and lupus, or cancer.
Symptoms & Signs of Chronic Inflammation:
- Persistent soreness, swelling, and heat.
- Low-grade fever or subjective fever.
- Body rashes.
- Joint swelling and pain with loss of function.
- Swollen lymph nodes.
- Excessive mucus secretion.
- Fatigue and low energy even when getting enough sleep.
- Brain fog.
- Uncomfortable abdominal bloating, food sensitivities, changes in the stool.
The chronic inflammation theory is new to allopathic medicine, but naturopathic doctors have a broader sense of how the body functions and suspected chronic inflammation was behind many of our modern diseases.
Conditions Linked to Chronic Inflammation:
- Alzheimer’s disease
- Cancer
- Cardiovascular disease
- Chronic hepatitis
- Chronic pain
- Chronic rhinosinusitis
- Depression
- Endometriosis
- IBS/IBD
- Insomnia
- Lupus erythematosus
- ME/CFS
- Metabolic disease
- Obesity
- Periodontal disease
- Rheumatoid arthritis
Blood Tests to Detect Inflammation
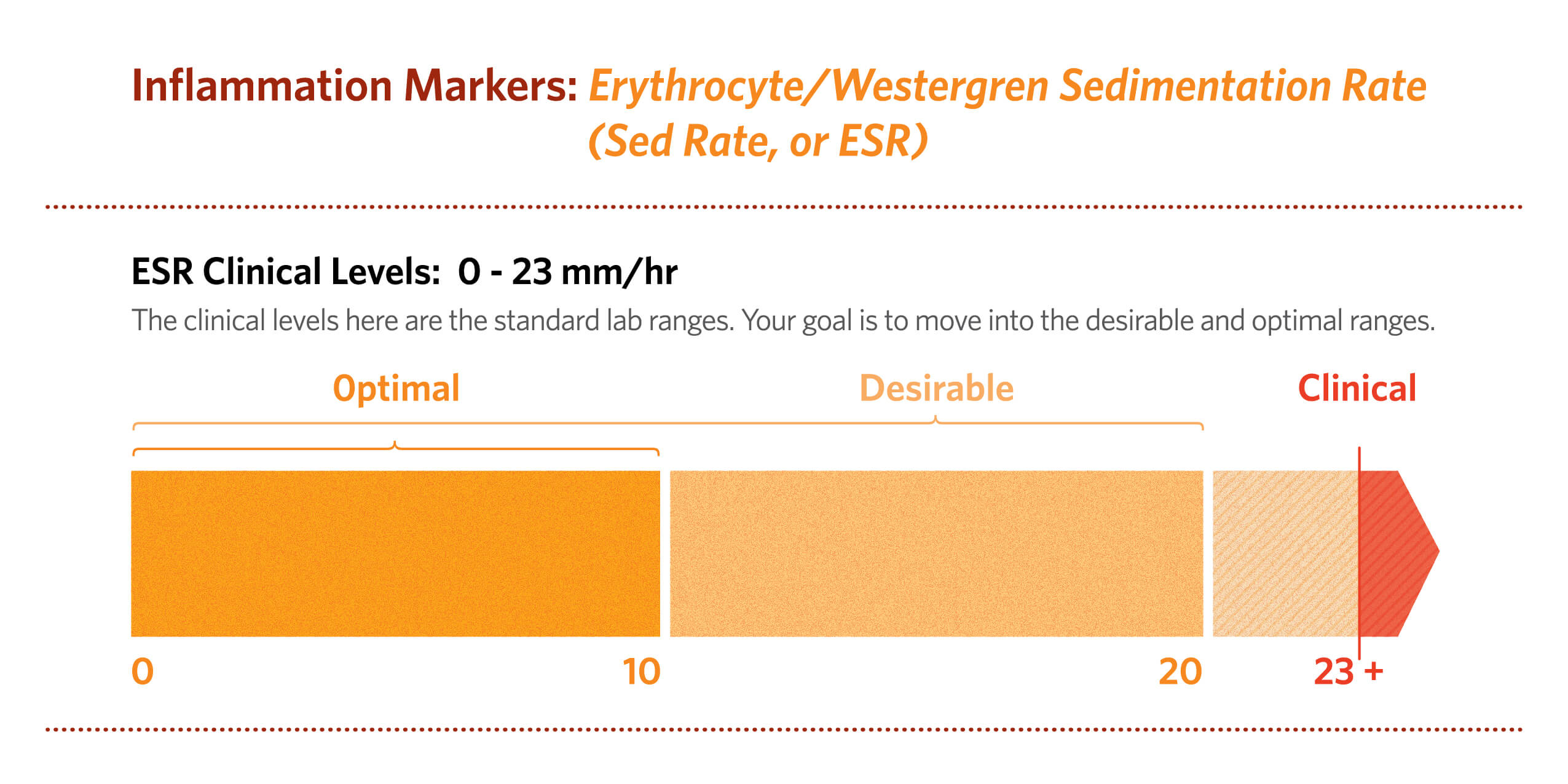
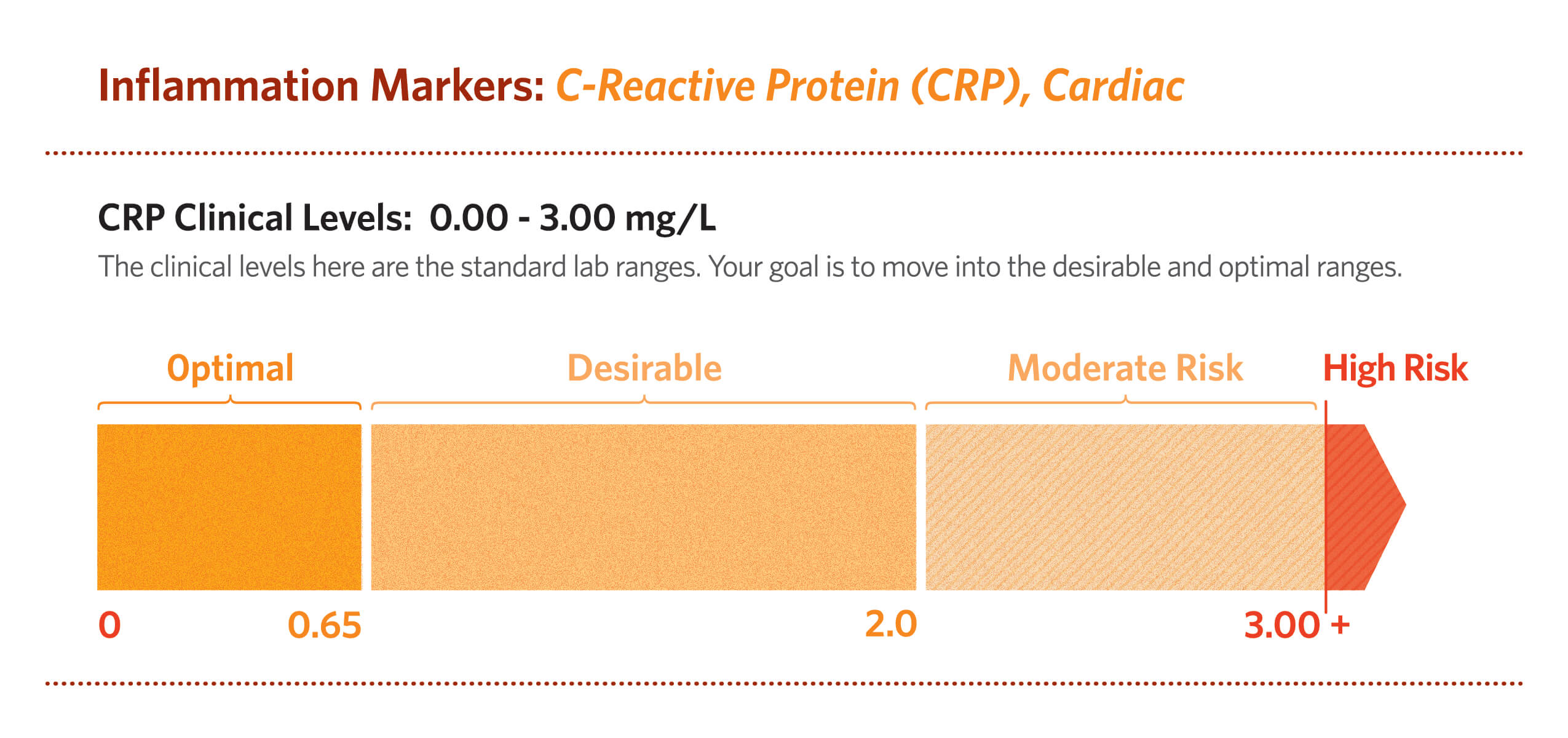
Three standard blood tests help detect inflammation. If you have acute inflammation or active chronic inflammation, one or more of these become elevated. And the higher your results are, the greater the inflammation.
3 Common Inflammation Markers:
- Erythrocyte sedimentation rate (ESR or SED Rate)
- C-reactive protein (CRP) quantitative
- C-reactive protein, highly sensitive (CRP-hs or cardiac)
ESR is a non-specific marker for acute and chronic inflammation. It measures the rate that red blood cells settle in a test tube over time. The faster the sedimentation rate, the greater the inflammation. ESR is a reliable marker to track inflammation. It may be high in older people. But, many factors influence ESR, so you need other tests to determine the cause of inflammation.
Like ESR, elevated quantitative CRP shows non-specific inflammation in the body. It doesn’t rise in response to chronic viral infection. So, ME/CFS patients with underlying chronic latent viruses like EBV and HHV-6, have a normal CRP level. However, it’s high in acute bacterial infections, like Lyme disease. CRP is more sensitive than ESR, so a high quantitative CRP helps determine the severity of chronic inflammation. Levels between 10-40 mg/L suggest mild-to-moderate inflammation. A level over 100 mg/L signals active inflammation.
CRP-cardiac detects low levels of C-reactive protein from plaques in the arteries. Persistent elevation of CRP-cardiac increases your risk for cardiovascular disease. Another marker for vascular inflammation is lipoprotein-associated phospholipase A2 (Lp-PLA2). High CRP-cardiac and Lp-PLA2 signals active inflammation in your blood vessels.
Five Reasons Why You Need to Get Your CRP Tested
Case Study Continued
A few years after I treated Maryanne’s MRSA, she returned. At first, I thought the infection was back. But, her hair looked healthy. When I asked how I could help, she told me about another condition, one she hadn’t revealed when I first saw her.
She had chronic heart failure, along with high blood pressure and high LDL cholesterol. Her cardiac CRP-cardiac level had soared to 35 mg/L. According to her cardiologist, there were no drugs to bring the high CPR level under control.
“You must make big changes,” I said. “If you agree, I’ll work with you.”
“Do I have a choice?” she replied. “You’ll put me on carrot sticks and green juice, but I can handle it.”
I prescribed a healthy, balanced vegan diet for six months plus anti-inflammatory supplements. It’s difficult to make fundamental lifestyle changes. For Maryanne it was a process: relearning where and how to grocery shop, and classes in healthy cooking methods like steaming instead of pan-frying. And, she took supplements three times daily.
In three months, her CRP-cardiac was lower. Over the next two years, it progressively went down until it was 1.3 mg/L. Her cardiologist was so impressed; he now takes supplements for his heart health. For the last four years, Maryanne’s ESR stayed about 2 mm/hr, and her most recent CRP-cardiac was 2.2 mg/L.
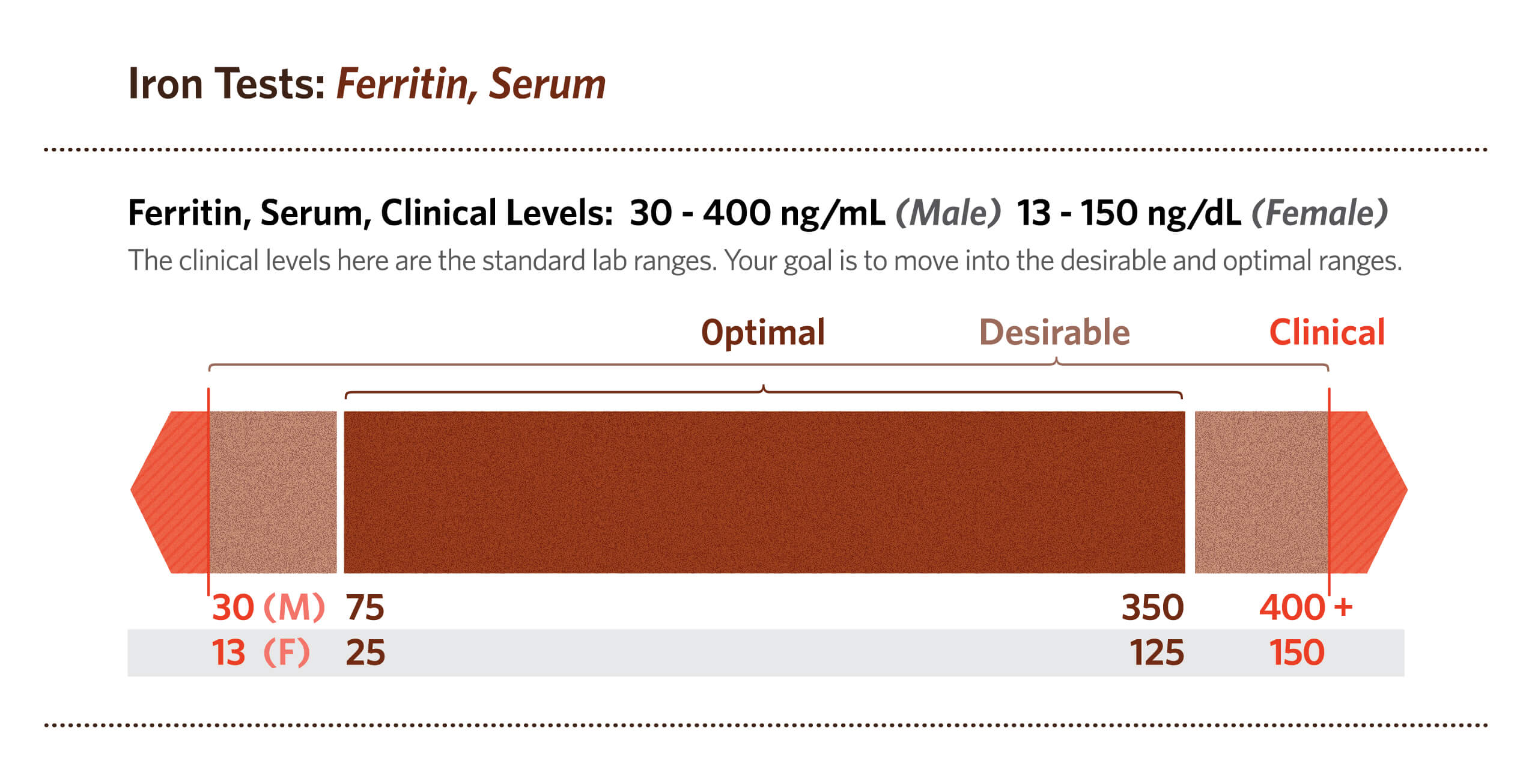
Additional Laboratory Markers of Inflammation
Because chronic inflammation is not associated with acute infection, your white blood cell (WBC) count may be normal. But, the WBC level and neutrophils increase with infection. And, during acute infection like when you have the flu, your body removes iron in your blood because invading microbes thrive on iron. When iron levels drop, ferritin increases. High levels of ferritin suggest inflammation associated with infection. However, high ferritin is also found in the blood of overweight people because obesity is linked to chronic inflammation. In these cases, CRP is also elevated. [1]
If inflammation happens in your liver, specific enzymes including alanine transaminase (ALT) and aspartate transaminase (AST) are high. If you have inflammatory bowel disease (IBD) like colitis or an infection in your intestines, lactoferrin in a stool test is high. But, lactoferrin is not high in irritable bowel syndrome (IBS).
Normal Inflammatory Levels Are Associated With Health
Your body modulates inflammation as part of the response to disease. A healthy lifestyle and normal weight reflect health and keep inflammation in check. Obesity is linked to chronic inflammation. Diet plays a role in systemic inflammation.
Overeating animal protein and unhealthy fats trigger inflammation. Overeating arachidonic acid (AA), an omega-6 polyunsaturated fatty acid, foods like poultry, eggs, and beef triggers inflammation. Adding more vegetables in your diet, or going vegan lowers AA and helps bring the inflammation down. Try a vegan diet for five months and remeasure your inflammation markers. The anti-inflammatory Paleo diet provides a healthier nutritional balance for long-term management of inflammation. Avoid all refined sugar to reduce inflammation. And, keep your total daily sugar level below 24 grams.
7 Lifestyle Tips To Prevent Inflammation:
- Maintain a healthy weight and body fat.
- Exercise regularly with moderate intensity.
- Stay cool by sleeping with a temperature between 64-69 degrees.
- Get 8-9 hours of restful sleep.
- Tend to your gut health.
- Avoid inflammatory-promoting foods.
- Don’t smoke.
Sleep and immunity are linked. The immune system affects restorative rest, and inadequate sleep alters resistance. For example, when you get sick from the flu, the tendency is to sleep more. Likewise, adequate restorative sleep is essential to manage low-grade chronic inflammation. [2]
Unbalanced microbiome biodiversity is linked to chronic inflammation. Bacterial overgrowth in the colon can trigger inflammatory bowel disorders like colitis. But, low-grade chronic inflammation is also associated with low diversity, not enough friendly gut bacteria factors in CFS and IBS. Eat more vegetables, get enough fiber, and take probiotics to improve gut health and lower inflammation.
Natural Medicine Lowers Chronic Inflammation

A 2018 review of natural products that dampen inflammation found polyphenol compounds like epigallocatechin 3-gallate (EGCG) in green tea effective in lowering inflammation. [3] I recommend EGCG as front line treatment for obese patients because it modulates inflammation and reeves metabolism.
Devil’s claw (Harpagophytum procumbens) is a South African plant used for arthritic pain and inflammation. Ginger (Zingiber officinale) is good for digestion, helps prevent cancer, is an antioxidant, and has anti-inflammatory properties. Curcumin (Curcumin longae) is a polyphenol compound found in the spice, turmeric. It’s an antioxidant and helps manage inflammation. Resveratrol inhibits inflammatory signaling pathways.
Many find that natural anti-inflammatories are not potent enough to control the pain associated with inflammation. In this case, you may need a synergistic group of natural products to reduce inflammation and restore the body to normal. For example, cold-water fish contain resolvins,[4] natural compounds found in Omega-3 fatty acids that support resolution of inflammation. Without resolution, inflammation becomes chronic.
At a Glance:
- Avoid refined sugar.
- Avoid refined carbs.
- Eat more green vegetables.
- Eat raw organic seeds and nuts.
- Get enough fiber.
- Eat polyphenol-rich plants.
- Take polyphenol supplements.
- Take anti-inflammatory herbal extracts including curcumin and boswellia.
- Eat more cold-water fish and take Omega-3 fish oil.
- Try phytocannabinoids.
- Take a low-dose aspirin daily.
- Get acupuncture.
If an anti-inflammatory diet, weight loss, and regular exercise don’t bring your inflammation markers lower, add natural anti-inflammatory supplements. If these don’t lower your inflammation markers enough, try cannabinoids from plants other than cannabis. Hemp is not the only plant that makes cannabinoids. You’ll find cannabinoids in echinacea and indole-3-carbinol derived from the cabbage family. If plants aren’t strong enough, take a low-aspirin daily and consider acupuncture.
Inflammation is part of the body’s natural defenses. It’s a signal to the immune system to repair damaged tissue. Over time—if you can’t rest because of work or study schedule and are stressed—even low-grade inflammation will cause tissue degeneration resulting in poor health. Chronic inflammation may shorten your lifespan. To be proactive about your health and longevity, test your inflammation markers.
References:
[1] Abidullah Khan, Wazir Muhammad Khan, Maimoona Ayub, Mohammad Humayun, and Mohammad Haroon, “Ferritin Is a Marker of Inflammation rather than Iron Deficiency in Overweight and Obese People,” Journal of Obesity, vol. 2016, Article ID 1937320, 7 pages, 2016.
[2] Luciana Besedovsky, Tanja Lange, and Monika Haack, “The Sleep-Immune Crosstalk in Health and Disease,” 28 MAR 2019.
[3] Andrade, P. B., & Valentão, P. (2018). “Insights into Natural Products in Inflammation. International journal of molecular sciences,” 19(3), 644.
[4] Charles N. Serhan, Bruce D. Levy. “Resolvins in inflammation: emergence of the pro-resolving superfamily of mediators,” J Clin Invest. 2018;128(7):2657-2669.


