How to Lower Chronic Inflammation with Gut Bacteria
My nature cure mentor, Dr. Bernard Jensen, was right. All disease starts in the gut.
| | Reading Time: 3 minutes
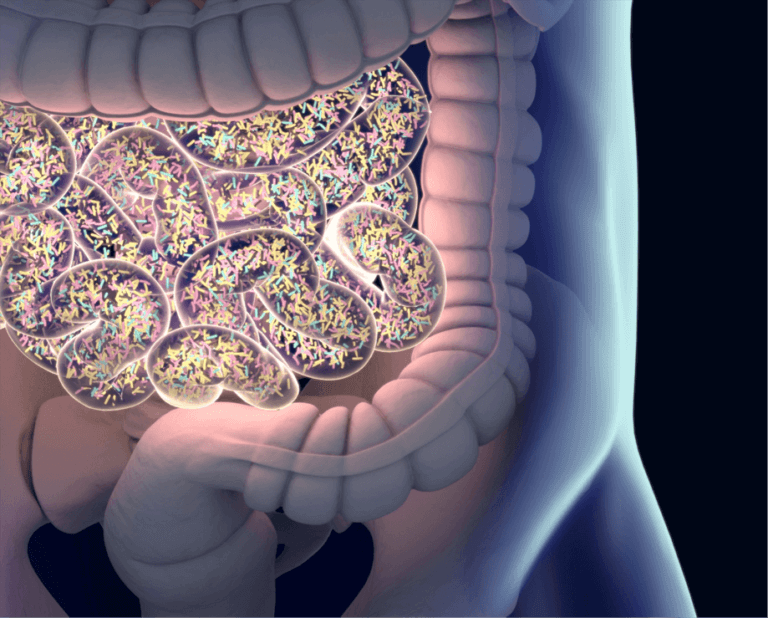
Science is proving that there is a link between gut endotoxins and chronic inflammatory diseases. Patients with leaky gut, irritable bowel syndrome (IBS) and inflammatory bowel diseases (IBD) like Crohn’s improve when they have less gut permeability, lower endotoxin load, and normalized inflammatory biomarkers like C-reactive protein (CRP). But the gut microbiome is an exceptionally complex environment. Is there a missing bacteria in the microbiome of patients with all these chronic diseases? Could it be F. prausnitzii?
My nature cure mentor, Dr. Bernard Jensen, was right. All disease starts in the gut.
A Common Gut Bacteria Is Associated with Chronic Inflammation
The first clue came in 2006 when Phillippe Langella discovered the anti-inflammatory properties of Faecalibacterium prausnitzii. Dr. Langella is a renowned microbiota researchers and director of Micalis in France, a company dedicated to understanding gut ecology.
Is F. prausnitzii the common biomarker of intestinal health? Does a deficiency cause chronic inflammation?
Too low levels of F. prausnitzii in the gut found with a stool test is associated with many common diseases including Inflammatory Bowel Disease (IBD), irritable bowel syndrome (IBS), diabetes, asthma, eczema, mood disorders, and obesity. Chronic inflammation is a common element of all of these conditions.
One of the most abundant bacteria in the human gut is F. prausnitzii. It’s a member of the Firmicutes phylum, one of the largest and most important groups of resident gut bacteria.
Microbial imbalance in the gut composition leads to dysbiosis. When too many harmful bacteria outnumber positive ones, dysbiosis sets the stage for chronic disease.
Selected Benefits of F. prausnitzii:
- Source of energy for maintaining intestinal health
- Manages inflammation
- Helps protect against glucose intolerance and type 2 diabetes
- Produces short-chain fatty acid butyrate necessary to prevent leaky gut
- Supports mucosal immunity
Unfortunately, a single F. prausnitzii probiotic is not available. But, judging by the strength of the research since 2006, look for next-generation probiotics including F. prausnitzii
Prebiotics remain the best way to support your colonies of F. prausnitzii. But remember that oat and wheat bran are often used in prebiotic formulas, as is corn starch. You absolutely cannot take these fibers if are on a lectin-free or gluten-free diet, or experience allergic sensitivity to corn, oats, or wheat.
Legumes like lentils, lima beans, and even garden peas also support healthy intestinal flora. However, remember that legumes contain lectins. If you’re lectin-sensitive, cook beans and peas well.
Prebiotics That Support F. prausnitzii:
- Apple pectin
- Arabinoxylan oligosaccharides (AXOS)
- Fructooligosaccharides (FOS)
- Galactooligosaccharides (GOS)
- Inulin
- Sumac-sorghum
Arabinoxylan supports the gut microbiome and protects F. prausnitzii. However, most commercial arabinoxylan comes from wheat bran. Instead, choose the Japanese form Rice Bran Arabinoxylan Compound (RBAC) made from rice bran and Shitake mushroom extract.
Additional ways to support F. prausnitzii include modified fasting, and taking vitamin B2 (riboflavin), calcium d-Glucarate, and grape seed extract.
A 2015 study found that the probiotic Bacillus coagulans GBI-30, 6086 supports healthy F. prausnitzii populations. Marketed as Ganaden BC30, this probiotic survives the trip from mouth to gut 100 times better than most other probiotics30.
The large intestine is devoid of light and oxygen. Yet, bacteria thrive on energy from food remains and prebiotics. Researchers found that F. prausnitzii organisms are highly sensitive to even small amounts of oxygen. Adding the antioxidant supplements glutathione and cysteine to prebiotics help protect F. prausnitzii from oxidative damage.
Supplement Prebiotics to Support F. prausnitzii:
- Riboflavin
- Calcium d-Glucarate
- N-acetylcysteine (NAC)
- Glutathione
You can order these and other supplements reliably from Wellevate.
F. prausnitzii the common biomarker of intestinal health. Dysbiosis is associated with a deficiency of this bacteria. Improving F. prausnitzii status with diet, prebiotics and nutritional supplements help restore gut imbalances and lower systemic inflammation.