What You Need to Know About Getting a Flu Shot in 2024
| | Reading Time: 10 minutes

As of early fall 2024, flu activity is minimal across the US. But, if it worsens in the winter, are you protected if you had a flu shot in September? Is it too late to get vaccinated now, or is it better to wait to see how active this flu season gets in the fall? Should you get vaccinated at all?
I’ve said this before: “I’m not an anti-vaxxer.” Some vaccines save lives. However, anti-vaxxers’ concerns are valid. Not all vaccinations are safe all the time, and not every vaccine protects everyone from infection. It’s time to review the safety and value of influenza immunization. Let’s take a closer look at the current flu shot.
But first, let me be clear: influenza is a dangerous, sometimes fatal, respiratory viral infection. We had some tough influenza seasons. The 2017-2018 flu season was among the deadliest in recent memory. There were over 900,000 people hospitalized, and 80,000 died in the U.S.: that’s about 4,000 American deaths each week.
And during the COVID-19 Pandemic, it was complicated by surges in SARS-CoV-2 infections. COVID is still around. It’s surging again, with the highest number of infections since 2022. Several viruses cause a fever and similar respiratory symptoms to the flu.
If you have respiratory symptoms but don’t know what virus is making you sick, you can get a blood test from a single sample to test for influenza A and B, respiratory syncytial virus (RSV), and SARS-CoV-2 (COVID).
What have we learned from a severe influenza season? The CDC answers that more people should get a flu shot. But there’s more to beating the flu than vaccination. In my book, Beating the Flu, I wrote extensively about managing influenza. In this article, I address the benefits and downsides of the flu shot.
The Influenza Virus Is Complex and Challenging
- Influenza is seasonal. Typically, flu cases in the Northern Hemisphere start in September and October, peak between mid-November, and the tamper off in February. However, that pattern is changing. Some year’s flu hits hardest in late January and maintains peak levels through March. Some don’t wind down until late May. If you get a flu shot in August or September, and flu infections don’t surge until February, you’ll need a second shot.
- The influenza virus is dynamic. Seasonal influenza constantly changes, evolves, and spreads across different animal species, not just infecting humans. There are three main types: Influenza A, B, and C. Influenza A is subdivided into H and N subtypes, creating 144 possible combinations. The evolutionary path keeps going, and new flu variants always emerge.
- Influenza activity varies from year to year. Typically, influenza originates in the Southern Hemisphere and spreads globally in just a few months. It’s active for several months, reaches a peak, and then dissipates until next year’s fall and winter season.
Common Concerns & Myths Associated with Influenza Vaccines:
- Egg allergy reactions – Unlikely. Though a few reports of hives after a flu shot occurred in people without egg allergies. However, because most influenza vaccines are produced in chicken eggs, those with severe egg allergy may react. But, the amount of egg protein in the vaccine is minimal and not considered a risk. If you have a known egg allergy, two egg-free, recombinant vaccines are available: Flublok and Flucelvax.
- Other reactions – Possible but not likely. Common reactions include fatigue, headache, muscle or joint aches, and soreness or swelling at the injection site. I recommend resting for a few hours after immunization. Arm soreness can last a few days. It’s common and normal and means your body’s immune system responded to the vaccine.
- Thimerosal (mercury) poisoning – Single-dose vials, pre-filled syringes, and flu vaccine nasal sprays don’t contain the preservative thimerosal.
- Increased susceptibility to other respiratory infections – Not likely.
- The need for annual shots for life is accurate, but this is a large part of the controversy. The concern is about cumulative effects. Since the influenza virus constantly evolves, researchers must develop new matching vaccines.
- Need for increased doses for those over 65 years – True, older people need a flu shot that’s four times stronger to prime an immune response to protect them from severe consequences of infection.
- Low effectiveness – True, effectiveness varies at best between 40-60%, but sometimes as low as 10%.
Does A Flu Shot Protect Against Seasonal Influenza?
In some years, the flu shot is almost ineffective. For example, the CDC claimed the 2017-2018 Trivalent Vaccine for Influenza A(H1N1), A(H3N2), and B was 40 percent effective. However, it was only 25 percent effective against the robust H3N2 strain, which made people so sick. Other sources contradict the CDC’s claims. A study at Rice University found the vaccine less than 20 percent effective. (Bonomo & Deem, 2018) And in Australia, the vaccine was only 10 percent effective against H3N2. (Sullivan et al., 2017)
Even if influenza vaccines work half the time, it still doesn’t prevent catching the flu. However, if you do get sick, your symptoms may be milder. It might keep you out of the hospital. And, if you’re at high risk from complications from the flu, such as pregnant women, older people, and those with compromised immunity, it could make a difference in surviving the flu.
The case I make for my patients is that it’s individual. Hospital workers and schoolteachers have high exposure and may benefit from getting a flu shot. Most states do not require teachers to get vaccinated.
A Closer Look at Flu Shot Myths:
- You can get influenza from a flu shot. That’s not true with current inactivated vaccines. However, some people could experience immune reactions similar to flu symptoms, including fever, fatigue, and sometimes nausea and vomiting. This is likely why people think they caught the flu from the shot.
- You could get Guillain-Barré syndrome, a severe neurological disorder. It’s rare, but it could happen. In 1976, a Swine Flu pandemic scare loomed, and 45 million people in the U.S. received vaccinations. More than 450 people contracted Guillain-Barre syndrome. Much of the antivaxx concerns and hesitancy of people to get the flu shot stem from 1976. Influenza vaccines are safer now. The CDC estimates one or two cases of Guillain- Barré occur per million doses of the influenza vaccine.
- Flu shots for pregnant women cause birth defects or autism. Not true. There’s little evidence that the inactivated influenza vaccine affects a fetus. However, a respiratory infection during pregnancy can stress the mother’s lungs and heart. So, preventing catching the flu during pregnancy is essential. However, though there’s no concrete evidence that the mother’s flu shot helps or harms her fetus or newborn, I recommend that pregnant women prevent infection and avoid getting vaccinated.
- Everyone needs a flu shot to create “herd immunity.” Mostly true. The idea is that during a bad flu season, like in 2017-2018 or a pandemic, the more people vaccinated, the less chance of spreading the infection. The theory is correct but may only sometimes work in some cases.
- Flu shots work for everyone and all ages. That is not entirely true. The flu shot works best in healthy adults, teens, and older children. Infants under six months shouldn’t get vaccinated. The immune systems of children under two years and adults over 65 years do not respond as well to immunization. Seniors need a higher-dose vaccine or one with additional ingredients to stimulate an immune response. Fluzone High-Dose Quadrivalent vaccine, Flublok Quadrivalent recombinant flu vaccine, and Fluad Quadrivalent adjuvanted flu vaccine are the recommended shots for those over 65.
- The strongest are the most vulnerable. Partially true. The immune system can react aggressively toward influenza infection, triggering severe symptoms, especially in younger adults. However, that age group is not singled out as having more reactions to the flu shot.
- The flu shot is ineffective. Partially true. Scientists divide influenza viruses into four main types: A, B, C, and D (that doesn’t infect humans). Influenza A is made up of numerous strains. New types emerge all the time. No one knows how many variants there are or could be, but it’s a lot. Countless is the word that comes to mind. Therefore, it’s unlikely we’ll ever have a “perfect” universal influenza vaccine, but that doesn’t mean it’s ineffective.
Influenza Vaccine Science Remains Flawed
Influenza virus biology is a massive field of study. I understand that it’s not easy for everyone to get vaccines right all the time. However, the main concern about influenza vaccine science is the rush to get vaccines on the market. Vaccines are a substantial annual income opportunity for pharmaceutical companies. Though the global market brings in billions of dollars, drug manufacturers claim they can’t make a profit. They only stand to make huge profits when more people are vaccinated. Some scientists claim the science is biased in favor of the manufacturers. That’s why I’m driven to educate people on how to prevent and manage viral infections. A proactive patient is a healthier patient.
A 2014 Cochrane Collaborative review found bias in scientific papers about influenza vaccine effectiveness. The report points out that the authors made claims unsupported by the data and favored industry-funded studies. The authors concluded that routine influenza vaccination as a public health measure for everyone needs more scientific evidence of efficacy or safety.
An updated review in 2018 found that inactivated influenza vaccines reduced the effects of the flu by 2.3% in adults. The authors were uncertain about the evidence for getting seasonal vaccines during pregnancy, stating that, at best, it provides minimal protection.
Do You Need a Flu Shot Every Year?
Besides its low performance, the annual flu shot policy concerns me the most. Other types of vaccines, like measles and polio, provide better coverage for these viruses. Lifetime protection from measles for children only requires two shots. One shot for polio grants 99 percent protection for 18 years. But for influenza, you must get a shot yearly for your entire life without guaranteeing effectiveness. Even when it works well, you only get average effectiveness of reduced symptoms that vary yearly depending on the influenza strain in circulation and your immune status. Could you do just as well with proactive prevention and early treatment?
Why Not Skip the Shot, Catch the Flu, and Treat It with A Drug?
There are a few antiviral drugs for influenza, but these don’t work well and are expensive. Even if they were effective, does the cost justify their use?
- Tamiflu (oseltamivir) only works if taken within a narrow window when you first develop symptoms. A 2009 report in the British Medical Journal found the evidence for the use of Tamiflu needed to be more cohesive, consistent, and less contradictory. A 2014 Cochrane Review found that oseltamivir shortened the duration of the flu by less than one day. The authors found no evidence that oseltamivir was any better than acetaminophen. A 2025 meta-analysis of the results of oseltamivir found that it only partially alleviated symptoms. Dosing is twice daily for five days.
- A new anti-flu drug, Xofluza (baloxivir marboxil), claims you only need one dose. Xofluza was developed in Japan by Shionogi. It acts at an earlier stage in the influenza virus replication cycle. When it works, it might shorten your sick time by one day.
Both drugs take about three days for effects to kick in, though Xofluza acts slightly faster than Tamiflu. Xofluza costs more than $150 for two tablets. Tamiflu costs about $50 for five days. Tylenol (acetaminophen) costs less than $9 for five days of symptom management.
Oscillococcinum, a homeopathic drug, may reduce the time you’re sick and lower the severity of symptoms. Garlic and echinacea are other common natural remedies for colds and the flu. However, my clinical experience finds they have mild effects, though studies don’t support their efficacy. However, many of my patients take them and report positive effects.
What You Should Look Out for During The 2024/25 Flu Season
This year’s variants are influenza A(H1N1) – a type of swine flu, and A(H3N2) – also a swine flu that quickly infects humans. It’s highly resistant to amantadine and rimantadine antiviral drugs used to treat the flu. High-risk patients, like the elderly, may consider antiviral medicines. Newer generation anti-influenza drugs include oseltamivir and baloxavir.
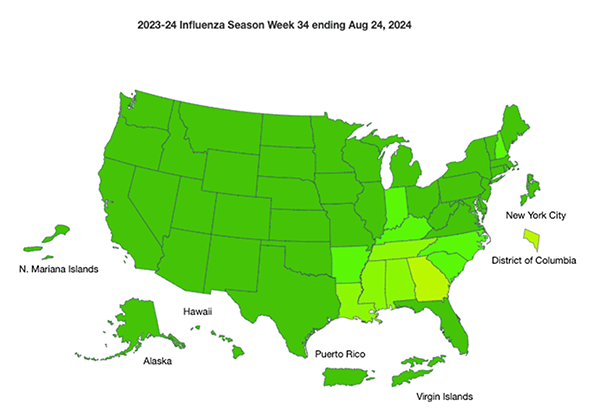
So far, this season’s influenza activity in the U.S. and Canada is low compared to other years. Public health statistics suggest a typical flu season. But that could change. To keep up with flu trends, CDC Influenza has a weekly report of seasonal activity.
Most of this year’s influenza vaccine is quadrivalent. It might be more effective than standard trivalent vaccines, but it costs more. Health insurance typically covers the cost of vaccination.
Booster doses, such as getting two or more flu shots, might be more effective. The CDC recommends two shots for children aged six months through 8 years. Those with immune deficiency conditions, like organ transplant patients and H.I.V., might benefit from two doses.
Fluzone, the high-dose trivalent flu vaccine, is four times the strength of the regular shot. It’s reserved for people over 65 years old. Fluzone should work better because it stimulates more antibodies against influenza viruses.
Considerations About Influenza Vaccination
I don’t have a “one-size-fits-all” answer about whether you shouldn’t get a flu shot. But you might consider the value of getting a flu shot for two reasons:
- Influenza infections are getting progressively stronger and spreading further, and flu season lasts longer, putting us at higher risk. Consider a flu shot if you’re at high risk for severe disease if you get influenza.
- We’re overdue for an influenza pandemic. Vaccination against a pandemic influenza strain could save your life. Keep up with the weekly influenza activity on FLUVIEW, the CDC website.
Herd immunity during a pandemic could significantly reduce the burden on hospitals and surge units and may reduce deaths. However, it takes at least 33 vaccinated out of 100 adults to prevent a single case of influenza. That means at least 70 percent need a flu shot to protect the population. On average, 46-48% of adults in the U.S. get a flu shot. In a worst-case pandemic scenario, city governments may mandate vaccination and prevent anyone not vaccinated from entering their city.
Vaccination may reduce your sick time and lessen the intensity of infection during a severe flu season, which could make a difference in your health and ability to work and keep you out of the hospital. Studies suggest that influenza vaccination prevents about 85,000 hospital visits for the flu every year.
Flu vaccination can save a child’s life. Pregnant women and their fetuses are more vulnerable to the consequences of influenza infection, so a flu shot might help avoid the worst. Still, I have reservations about universal flu shots for pregnant women and infants. And I don’t favor two doses for young children.
Exposing young children to too many vaccines, including annual flu shots, is risky. In 2014, the FDA approved a nasal spray for children, FluMist. In 2016, the FDA withdrew its recommendation because FluMist didn’t work.
Though largely ineffective for older people, who need a dose four times the average, vaccination may reduce hospitalization and deaths.
The flu shot’s protective benefits take about two weeks to work. The best time to get vaccinated is in the fall during a typical flu season, but late December or early in the New Year works during flu seasons that peak later and last longer.
Influenza vaccines have improved over the last two decades. They are proven safe when used as recommended by the CDC. However, I question the wisdom of annual flu shots from infancy to old age until scientifically proven to be effective.
Your best bet for not catching the flu is to avoid contagion and support healthy immunity.
References:
Bonomo, M. E., & Deem, M. W. (2018). Predicting Influenza H3N2 Vaccine Efficacy From Evolution of the Dominant Epitope. Clinical Infectious Diseases, 67(7), 1129–1131. http://doi.org/10.1093/cid/ciy323
Demicheli, V., Jefferson, T., Ferroni, E., Rivetti, A., & Di Pietrantonj, C. (2018). Vaccines for preventing influenza in healthy adults. Cochrane Database of Systematic Reviews, (2). http://doi.org/10.1002/14651858.CD001269.pub6
Dobson, J., Whitley, R. J., Pocock, S., & Monto, A. S. (2015). Oseltamivir treatment for influenza in adults: a meta-analysis of randomized controlled trials. The Lancet, 385(9979), 1729–1737. http://doi.org/10.1016/S0140-6736(14)62449-1
Jefferson, T., Jones, M. A., Doshi, P., Del Mar, C. B., Hama, R., Thompson, M. J., … Heneghan, C. J. (2014). Neuraminidase inhibitors for preventing and treating influenza in adults and children. Cochrane Database of Systematic Reviews, (4). http://doi.org/10.1002/14651858.CD008965.pub4
Sullivan, S. G., Chilver, M. B., Carville, K. S., Deng, Y.-M., Grant, K. A., Higgins, G., … Fielding, J. E. (2017). Low interim influenza vaccine effectiveness, Australia, May 1 to September 24 2017. Euro Surveillance : Bulletin European Sur Les Maladies Transmissibles = European Communicable Disease Bulletin, 22(43). http://doi.org/10.2807/1560-7917.ES.2017.22.43.17-00707
Yuan Y, Wang RT, Xia J, Cao HJ. Interventions for preventing influenza: An overview of Cochrane systematic reviews and a Bayesian network meta-analysis. J Integr Med. 2021 Nov;19(6):503-514. doi: 10.1016/j.joim.2021.09.001. Epub 2021 September 4. PMID: 34544670.
Follow My Twitter Feeds During Flu Season
Check Out My Blogs About Treating the Flu with Natural Medicines
You’ll find detailed information on treating viral illnesses, including influenza, in my books:
Viral Immunity and Beating the Flu.